Total hip arthroplasty (THA) is one of the most successful procedures in not only orthopaedics but all of surgery. With the dramatic rise in the number of THAs performed annually and the necessary focus on value-based care and cost containment, implant selection becomes a factor of interest, particularly given the vast number of implant choices for THA and their substantial cost variation.
In the December 15, 2021 issue of JBJS, Campbell et al. look more closely at implant selection, specifically whether implant selection at the time of THA affects (1) the odds of having inadequate improvement in patient-reported pain, function, and activity; (2) the failure to achieve a substantial clinical benefit (SCB) in pain; or (3) the failure to achieve a patient-acceptable symptomatic state (PASS) for pain and function.
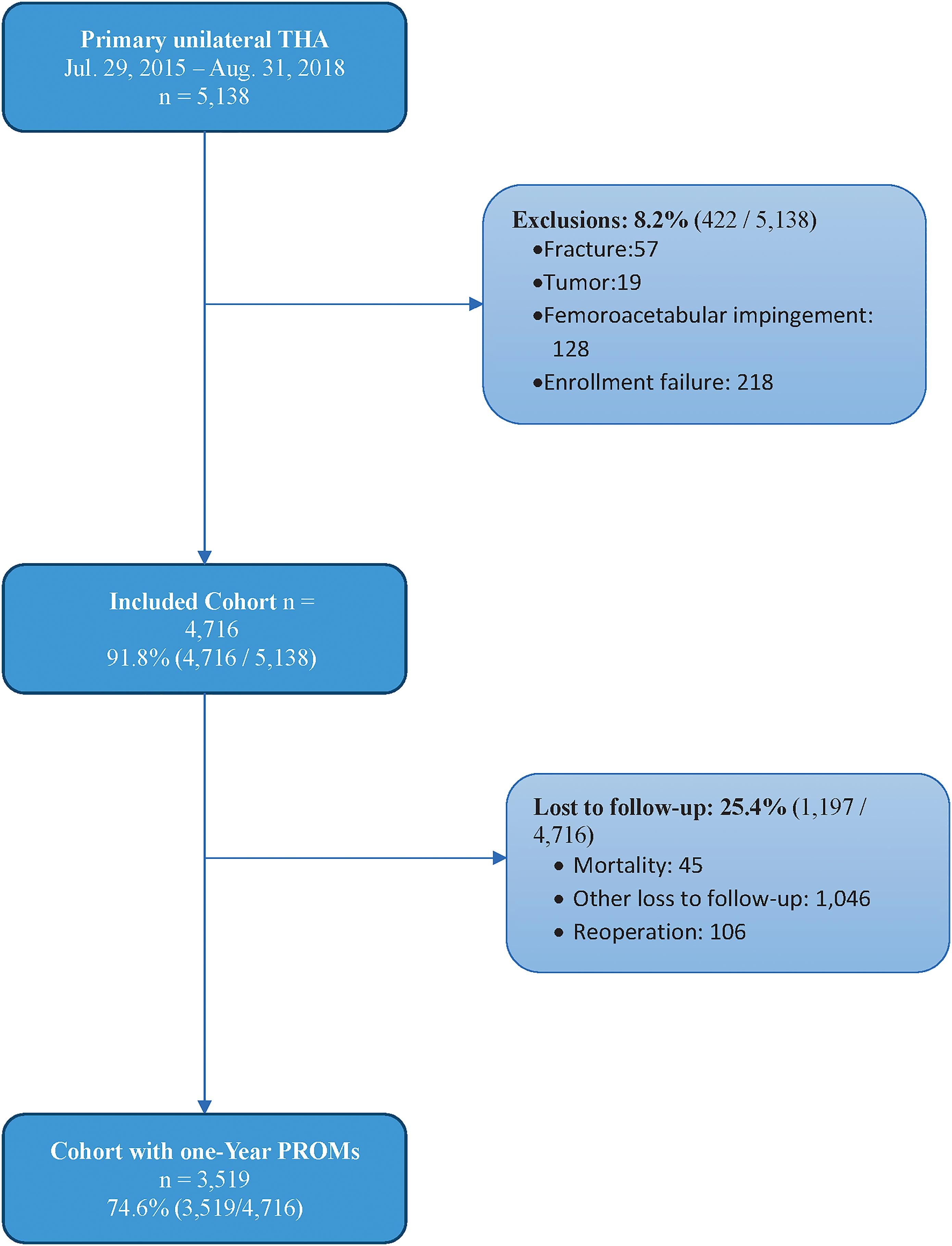
In this Level-III study, data were prospectively recorded for 5,138 patients who underwent primary unilateral THA between 2015 and 2018, as performed by 20 surgeons across facilities of a single medical system. Osteoarthritis was the main indication for surgery. Of these patients, 4,716 had baseline patient-reported outcome measures (PROMs), which included the Hip disability and Osteoarthritis Outcome Score (HOOS) pain subscore, HOOS physical function short form (PS), and the University of California at Los Angeles (UCLA) activity score.
The investigators also collected data on femoral stem geometry, femoral offset (although this was excluded from multiregression analysis due to incomplete data for a substantial number of cases), femoral head size, femoral head composition, acetabular component size, and acetabular liner type.
At 1-year follow up, the authors found:
- HOOS pain – Of 3,325 patients with available data, 3,214 (96.7%) met the minimal clinically important difference (MCID) and 2,621 (78.8%) met the SCB. Implant selection was not a significant driver of failure to attain the MCID or SCB based on multivariate logistic regression.
- HOOS PS – Of 3,006 patients with available data, 220 (7.3%) did not attain the MCID and 126 (4.2%) did not have any improvement. Implant selection was not a significant driver of not attaining the MCID.
- UCLA – Of 3,281 patients, 463 (14.1%) had inadequate improvement, as demonstrated mainly by homebound activity status (score of ≤3). Multivariate analysis showed that 36-mm femoral heads had lower odds of inadequate improvement compared with 28-mm heads (p = 0.003). There were no clinically important differences in femoral head composition or stem types.
- PASS – A total of 340 (10.2%) of 3,344 patients did not achieve a PASS, with no implant-related criteria as significant drivers.
The authors concluded that, although larger head size was associated with lower odds of inadequate improvement, the failure to reach an SCB in terms of HOOS pain and PASS were not dependent on the type of implant. So the question remains: do we really need such a plethora of implant choices? Could the range of available implants potentially be consolidated, and thus, cost variability be reduced? Additional high-quality, prospective research can help provide further answers as our community addresses value-based care while optimizing patient outcomes.
Matthew R. Schmitz, MD
JBJS Deputy Editor for Social Media