Topics of interest in orthopaedic trauma, including fracture fixation, pain management, and more, are highlighted in the new JBJS Guest Editorial What’s New in Orthopaedic
Category: Pain Management
Recent findings in spine surgery on topics such as lumbar facet arthroplasty, pain management, nicotine use, and more are presented in the new JBJS Guest
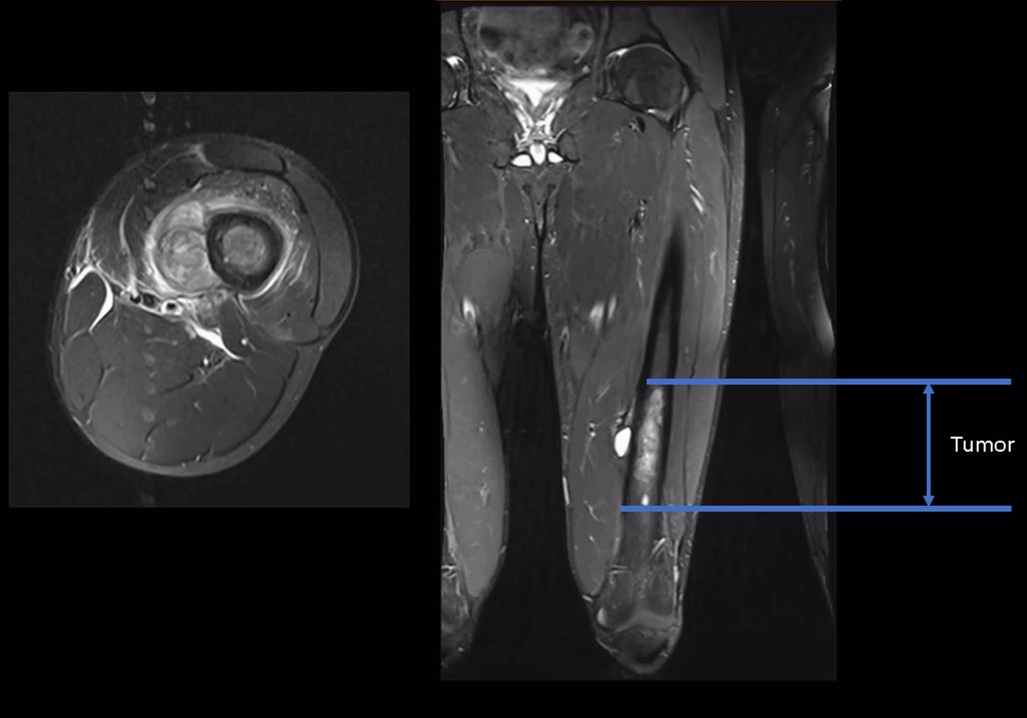
Recent findings in orthopaedic oncology and musculoskeletal tumor management are highlighted in the new JBJS Guest Editorial What’s New in Musculoskeletal Tumor Surgery. Here, we
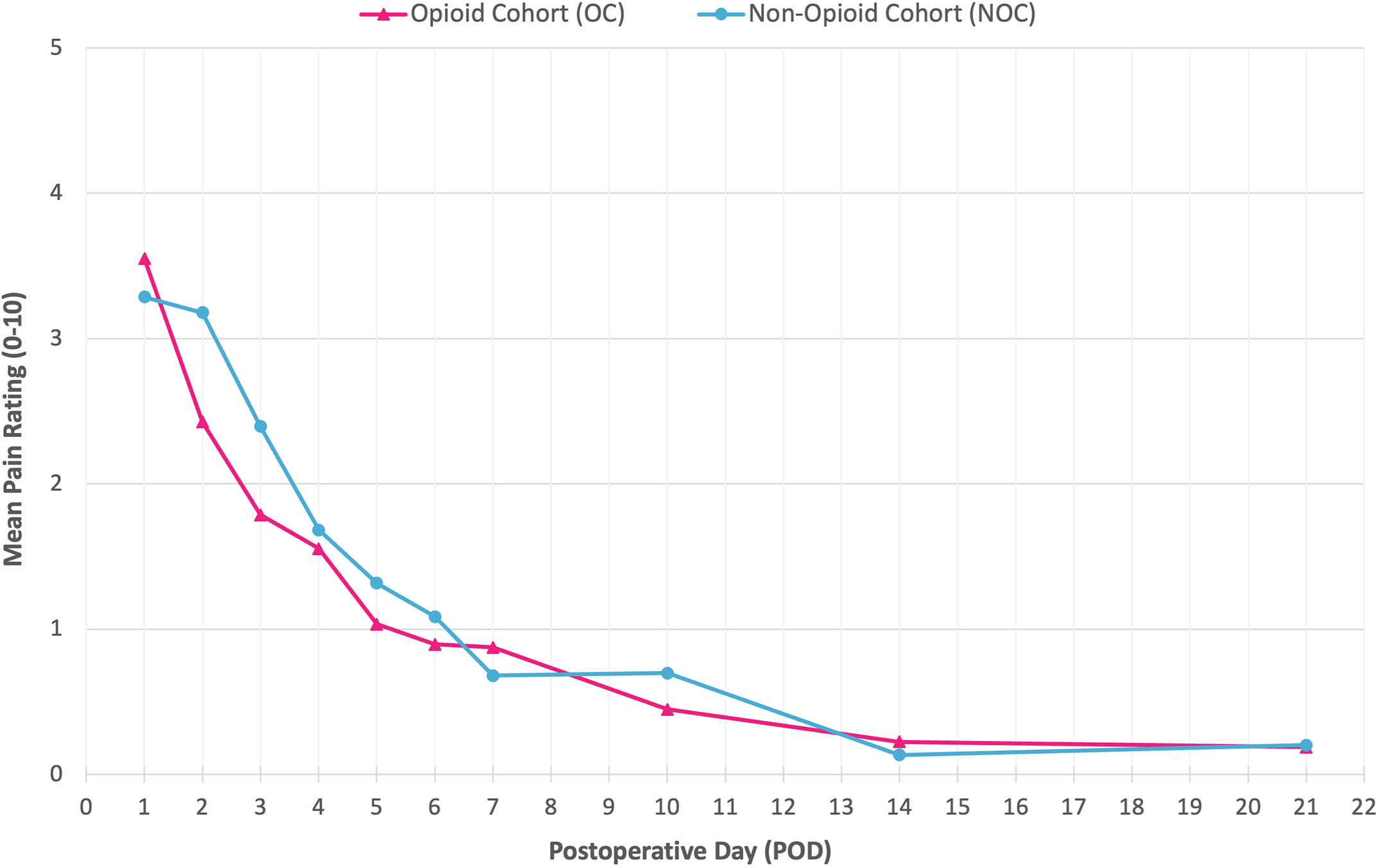
JBJS Deputy Editor for Social Media Dr. Matt Schmitz offers his thoughts on a new study comparing the efficacy of opioid and non-opioid analgesia following

Noteworthy findings regarding topics such as platelet-rich plasma injection, botulinum toxin injection, and microinvasive trigger-finger release, among others, are presented in the new JBJS Guest
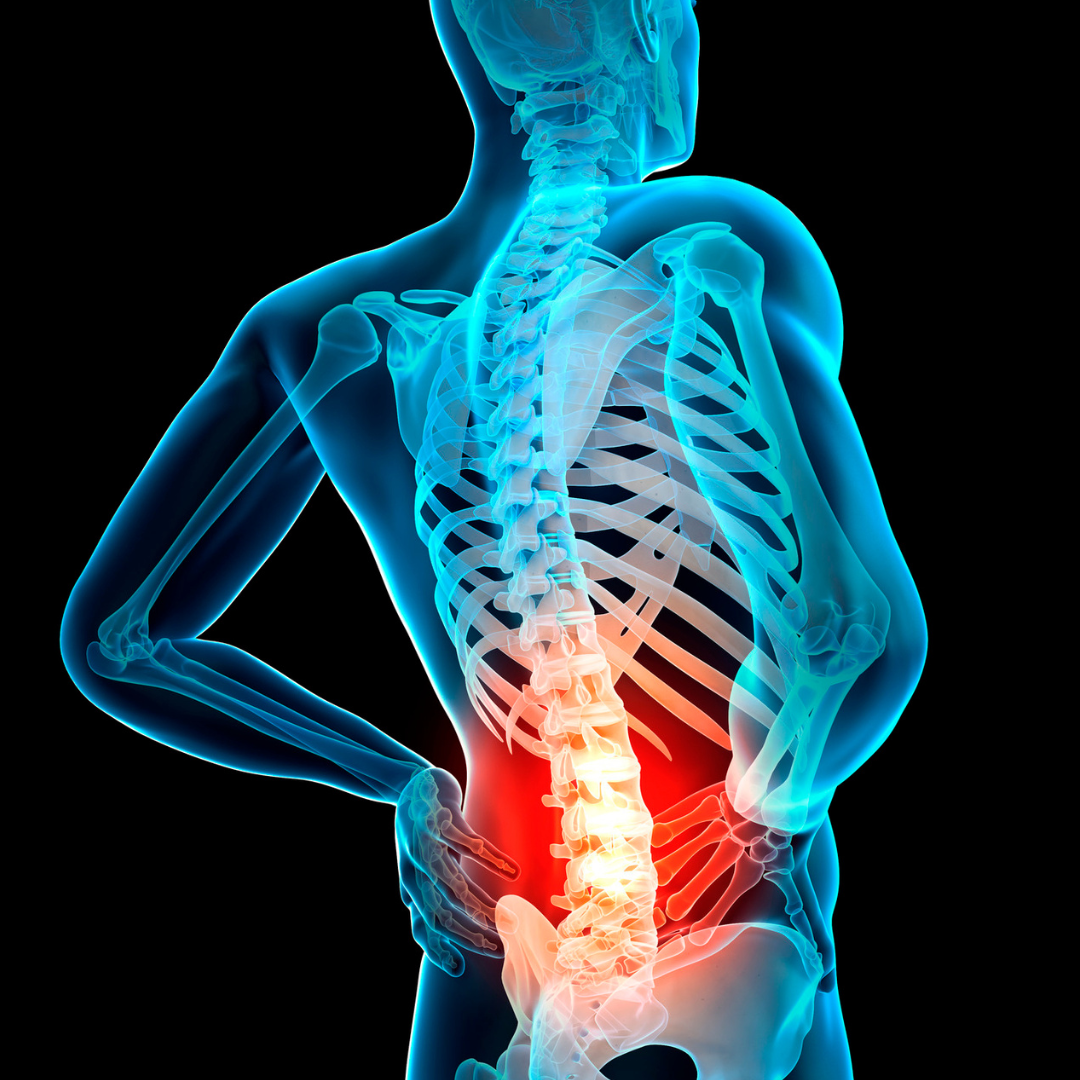
Recent studies on topics such as rates of lumbar spinal stenosis recurrence and the cost-effectiveness of early microdiscectomy are discussed in the new JBJS Guest

Topics of interest in the new JBJS Guest Editorial “What’s New in Sports Medicine” include opioid-sparing analgesia, risk of graft failure following meniscal allograft transplantation,
Symptomatic neuromas have long been a problem for amputees, interfering with prosthetic comfort and causing residual pain that often requires treatment. During the last 15
Corticosteroids are commonly used in total knee arthroplasty (TKA) to reduce pain and prevent nausea. But are the effects of steroids different when administered locally
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a