Key findings in sports medicine are highlighted in the new JBJS Guest Editorial What’s New in Sports Medicine. Here, we feature the 5 most impactful
Category: Sports Medicine
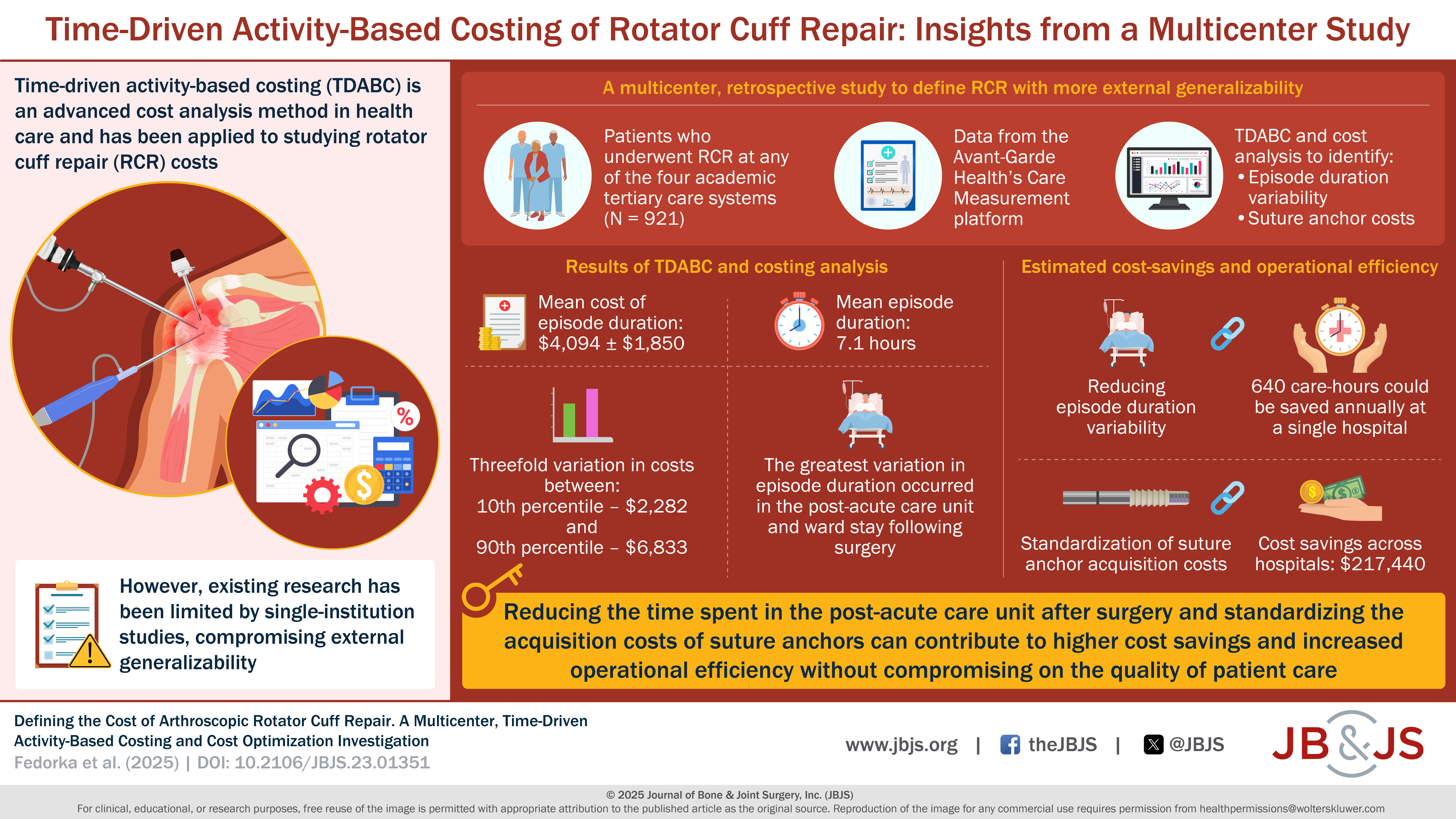
In a study now published in JBJS, Fedorka et al. evaluate the cost of rotator cuff repair (RCR) using time-driven activity-based costing (TDABC). This methodology,

New findings in musculoskeletal basic science are presented in the recent JBJS Guest Editorial What’s New in Musculoskeletal Basic Science. Here, we highlight the 5
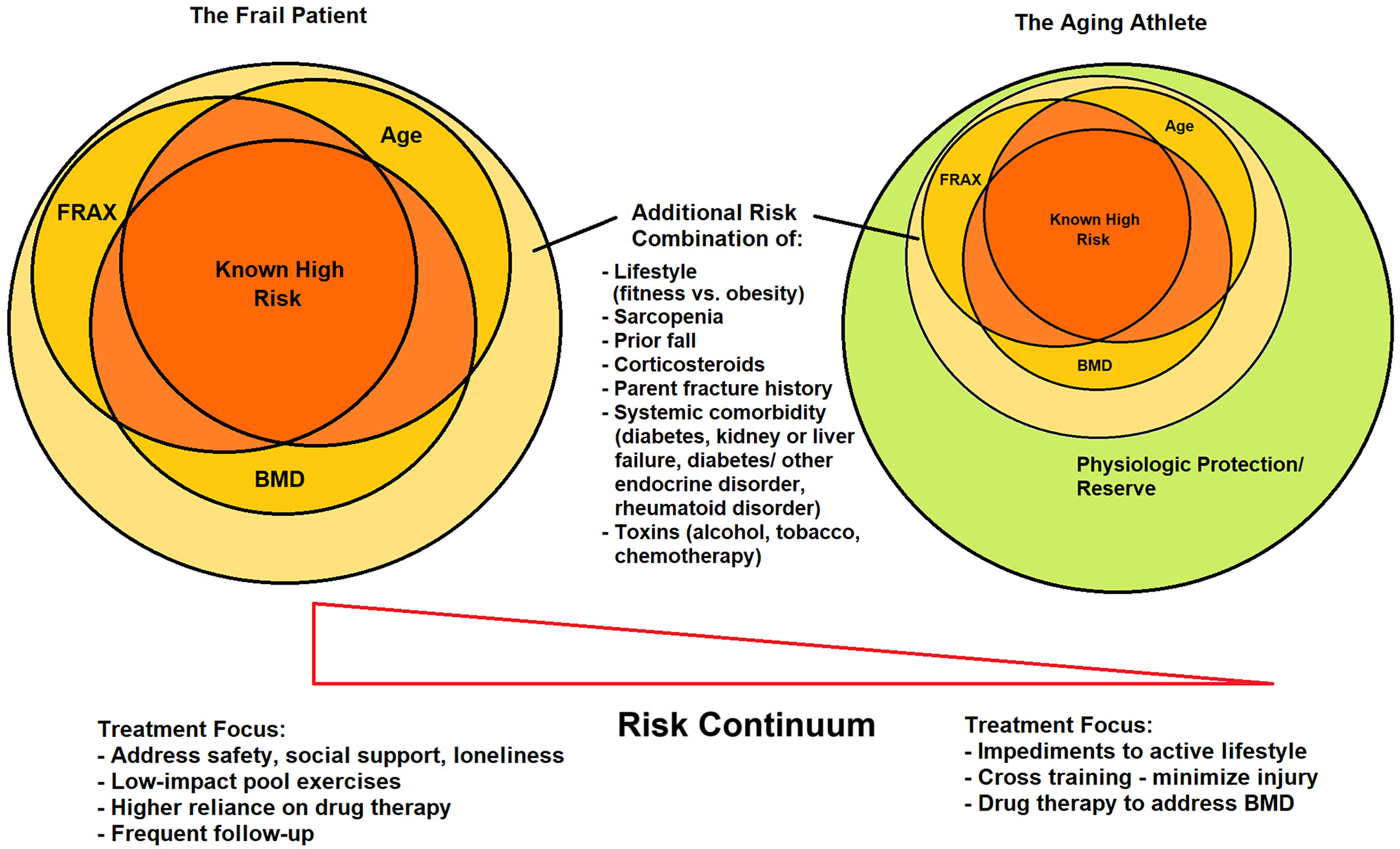
New insights regarding osteoporosis treatment and fracture prevention are highlighted in the recent JBJS Guest Editorial What’s New in Osteoporosis: Emphasis on the Aging Athlete.

Key findings in sports medicine on topics such as rotator cuff repair, anterior cruciate ligament (ACL) reconstruction, and more are presented in the new JBJS

Noteworthy findings regarding topics such as platelet-rich plasma injection, botulinum toxin injection, and microinvasive trigger-finger release, among others, are presented in the new JBJS Guest
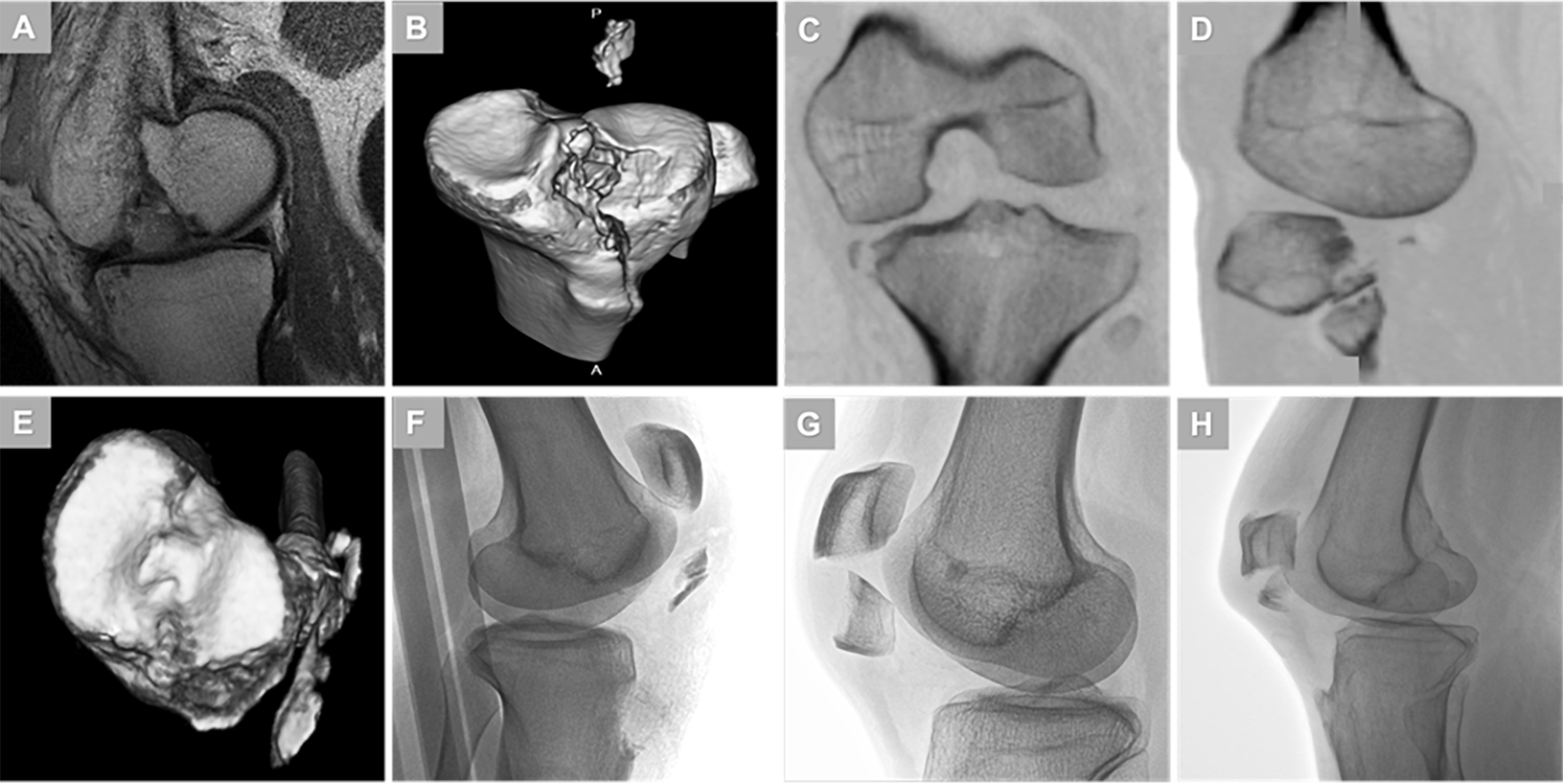
A new JBJS study establishes a consensus definition for fracture patterns within the Schenck Knee Dislocation V subcategory. Editor-in-Chief Dr. Marc Swiontkowski offers this perspective

This guest post comes from Jennifer Beck, MD, a pediatric sports medicine surgeon at Boulder Medical Center in Colorado and a member of the JBJS
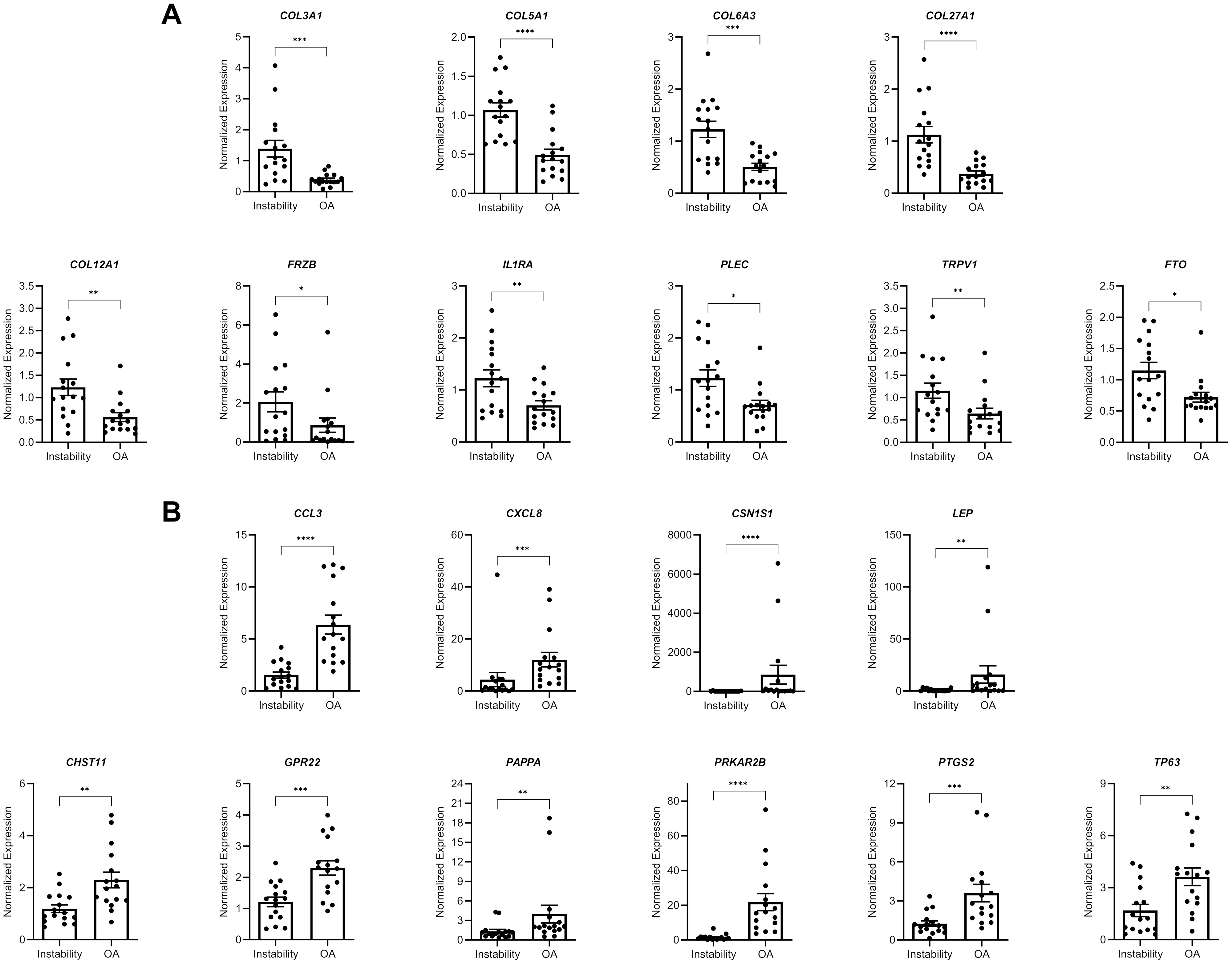
A new JBJS study presents novel data on gene expression in glenoid cartilage following shoulder instability. JBJS Deputy Editor for Social Media Dr. Matt Schmitz

A video summary is available with the new study by Birkenes et al. in JBJS: The Long-Term Risk of Knee Arthroplasty in Patients with Arthroscopically

