New research in hand and wrist surgery is presented in the JBJS Guest Editorial What’s New in Hand and Wrist Surgery. Here, we highlight 6
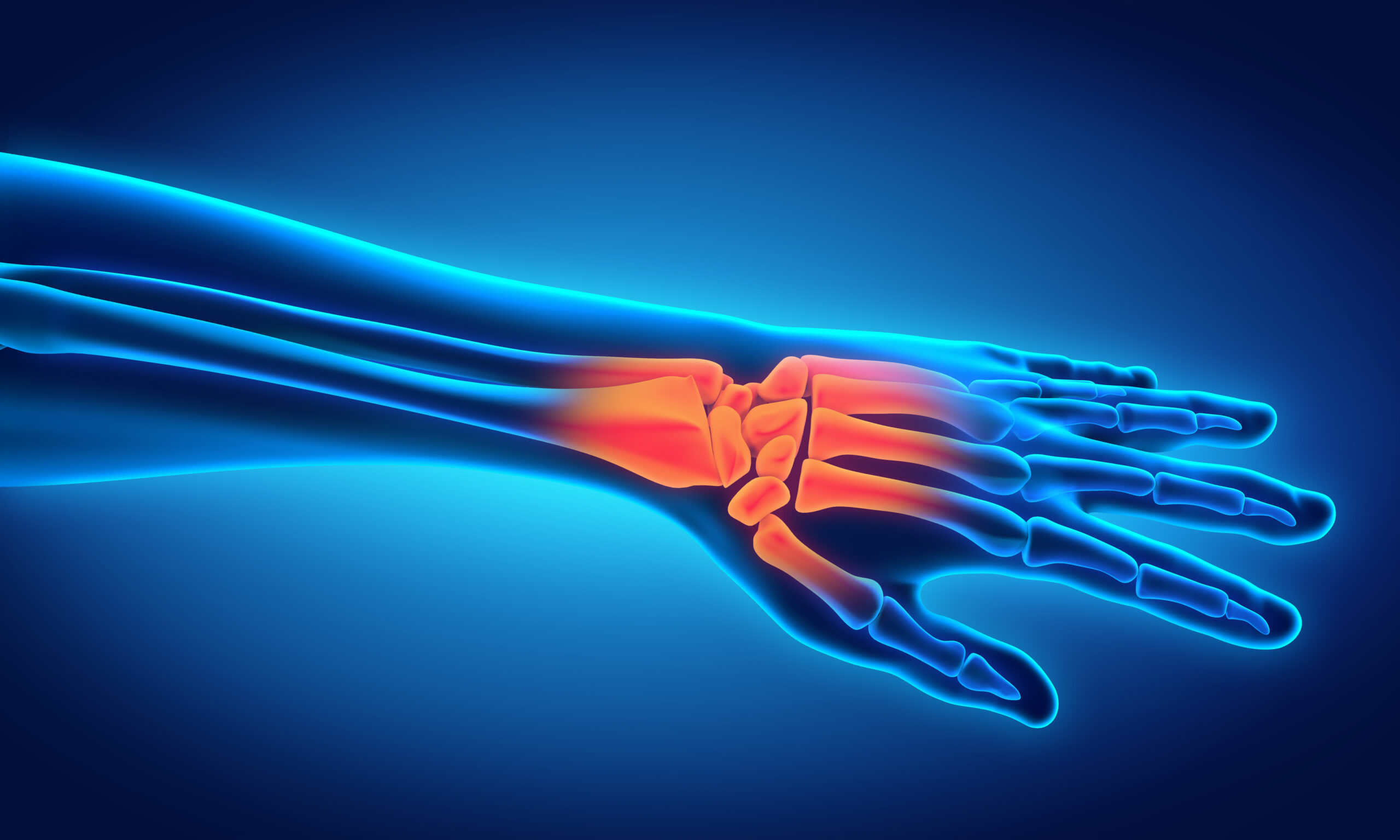
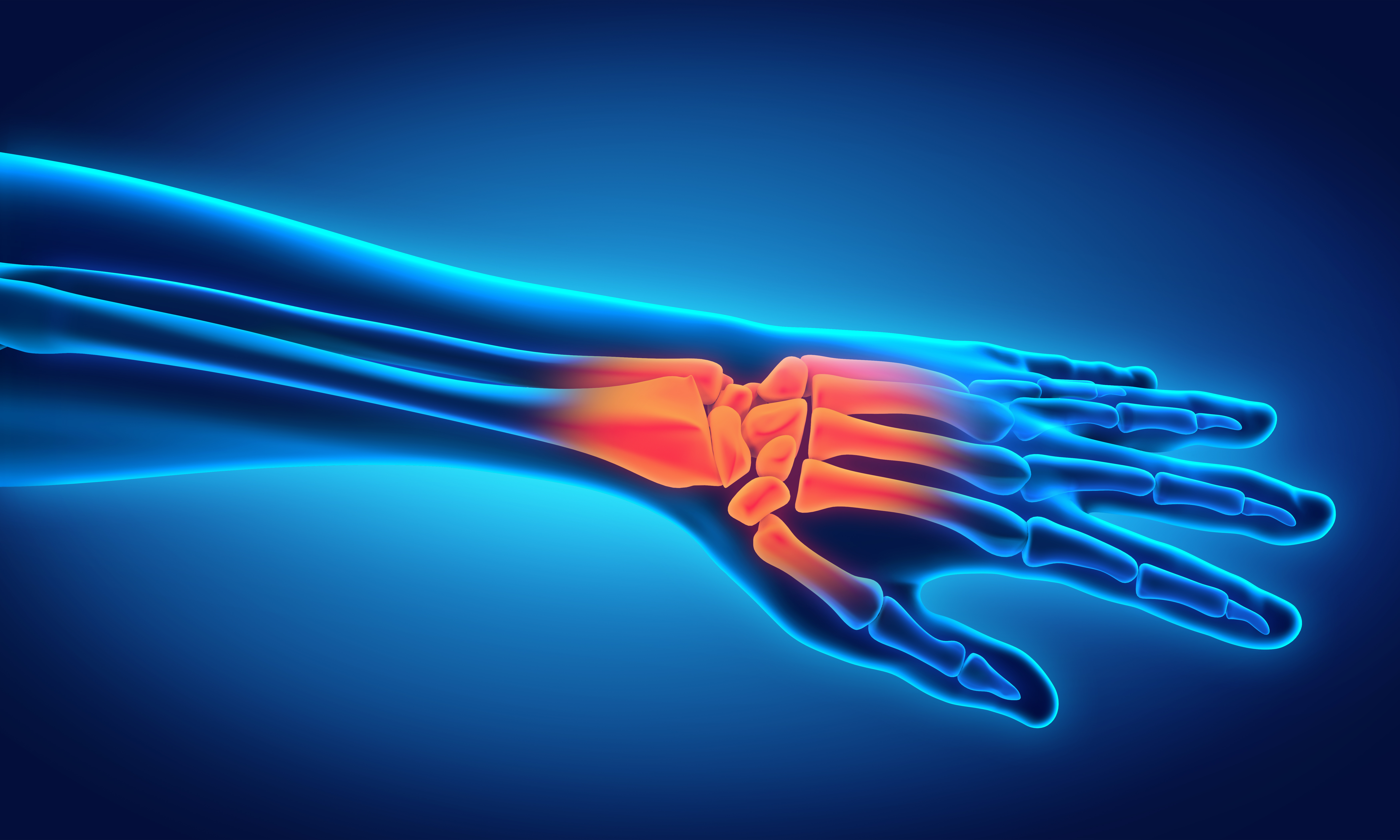
Category: Hand and Wrist
Topics of interest in orthopaedic rehabilitation, including platelet-rich plasma injections and novel minimally invasive techniques, are presented in the new JBJS Guest Editorial What’s New
Nonoperative treatment outcomes, the efficacy of waterproof cast protectors, and other topics of interest are presented in the new JBJS Guest Editorial What’s New in
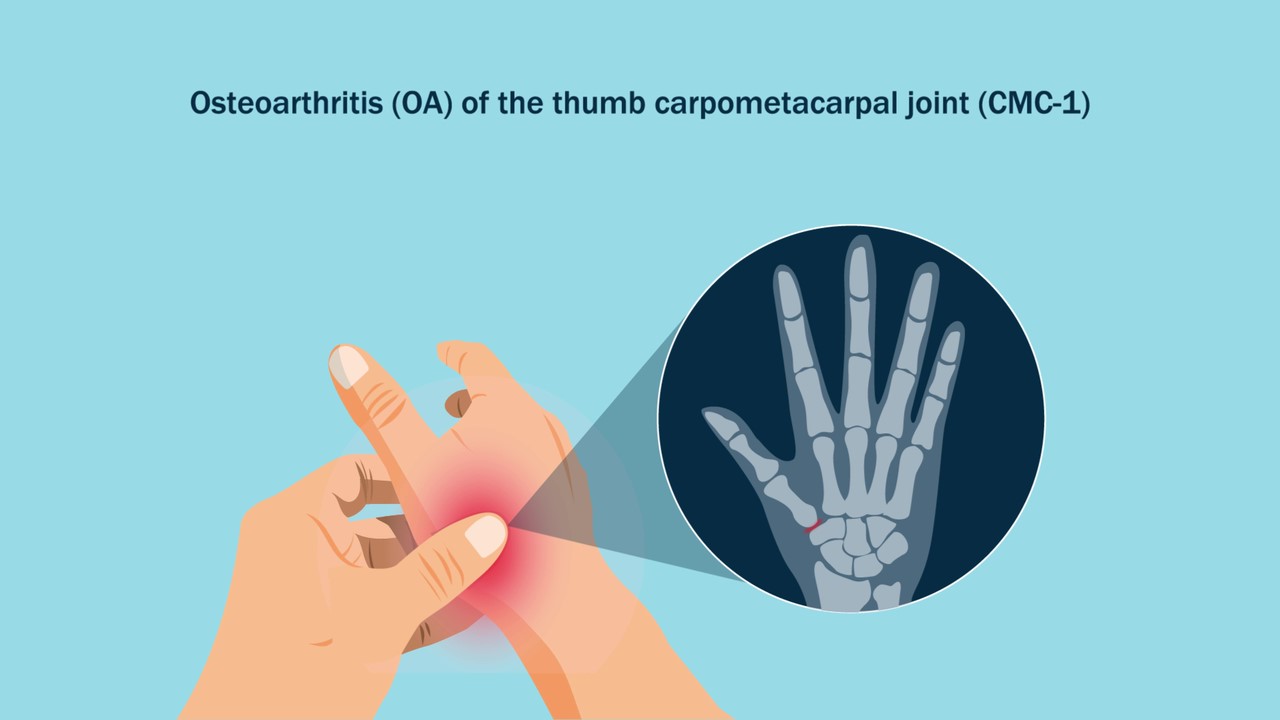
JBJS Editor-in-Chief Dr. Marc Swiontkowski shares this post on a new study in JBJS on outcomes of nonsurgical treatment of thumb carpometacarpal osteoarthritis at >5

Noteworthy findings regarding topics such as platelet-rich plasma injection, botulinum toxin injection, and microinvasive trigger-finger release, among others, are presented in the new JBJS Guest
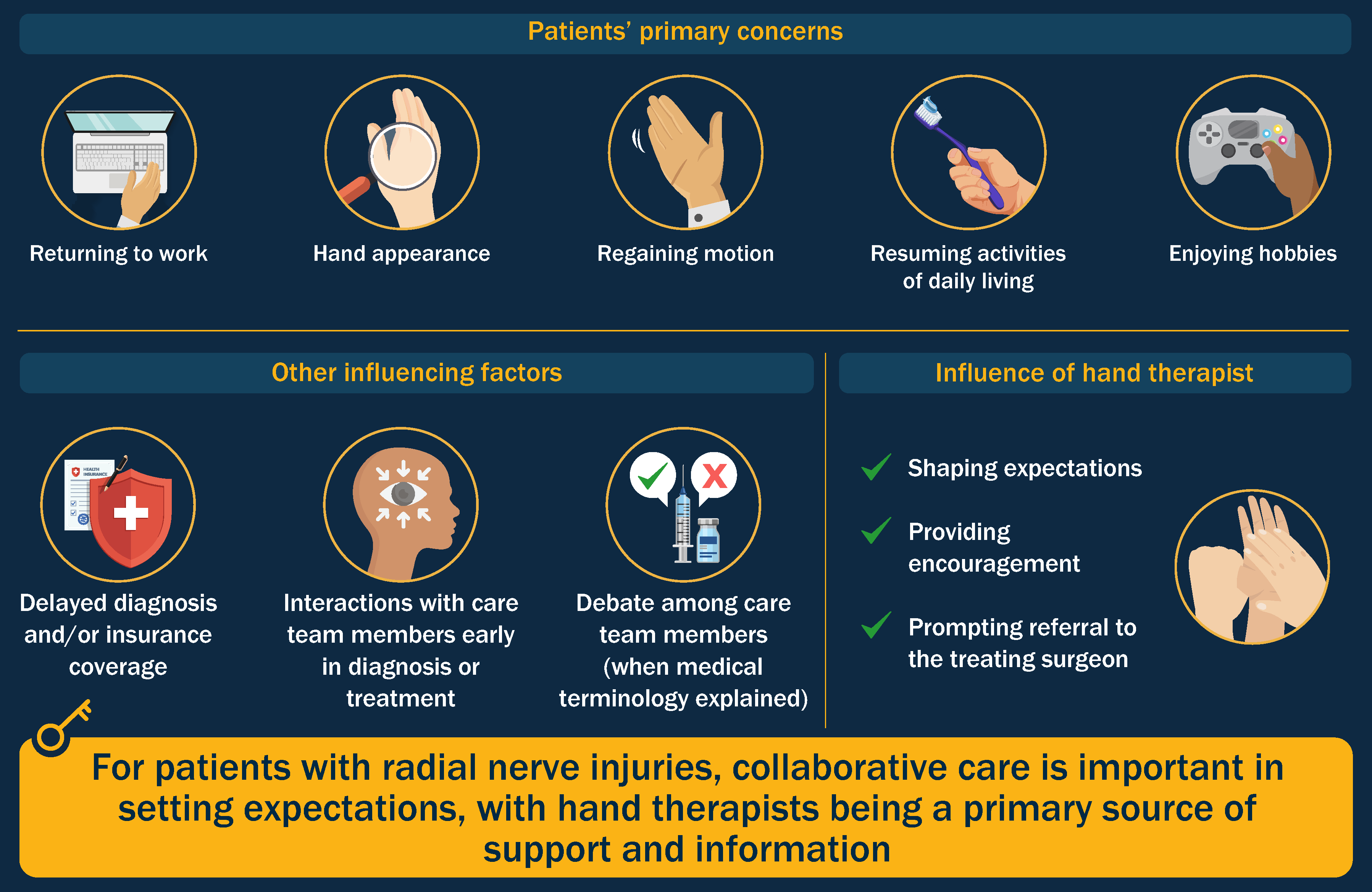
In this post, JBJS Editor-in-Chief Dr. Marc Swiontkowski discusses a new study evaluating patients’ treatment preferences and expectations in the management of radial nerve injuries.
The relationship between surgical site infection and preoperative corticosteroid injection for various procedures, findings on the long-term effectiveness of corticosteroid injection versus carpal tunnel release
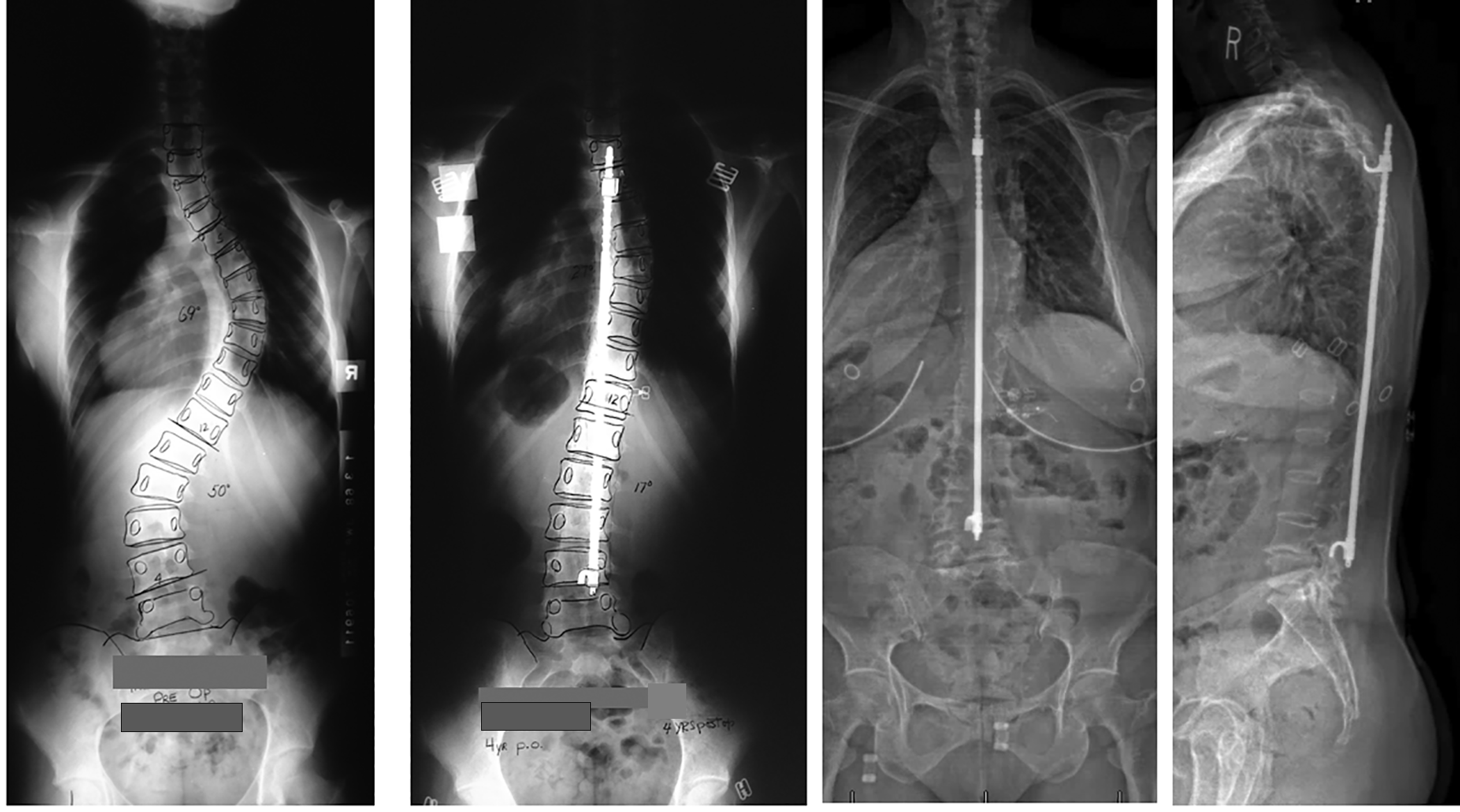
Patient outcomes ≥40 years after treatment for adolescent idiopathic scoliosis, return-to-sport rates following periacetabular osteotomy, and other important findings are covered in the new JBJS
Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, co-author

This OrthoBuzz guest post comes from Paul E. Matuszewski, MD, in response to a recent article in the New York Times. The ever-increasing importance of