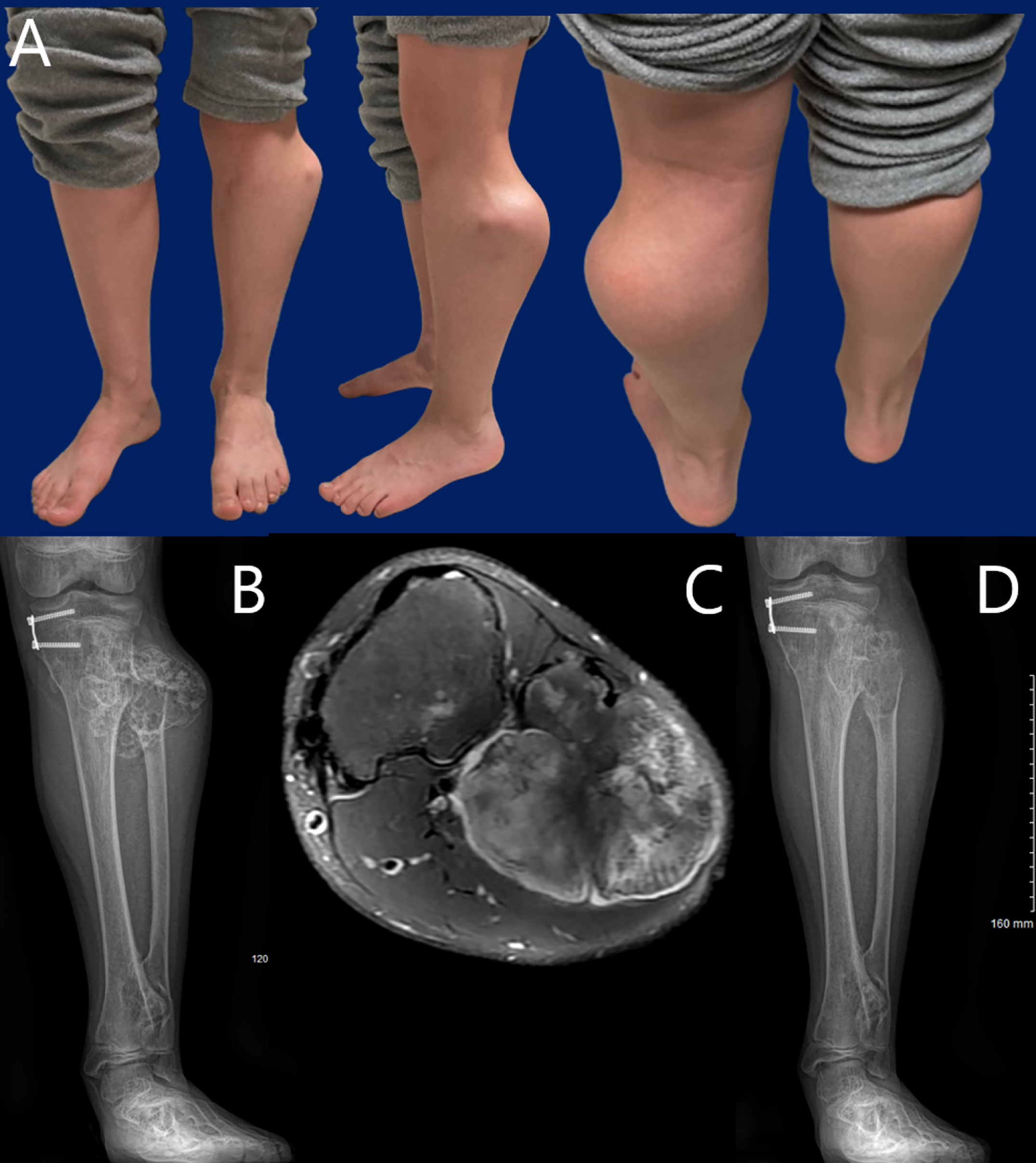
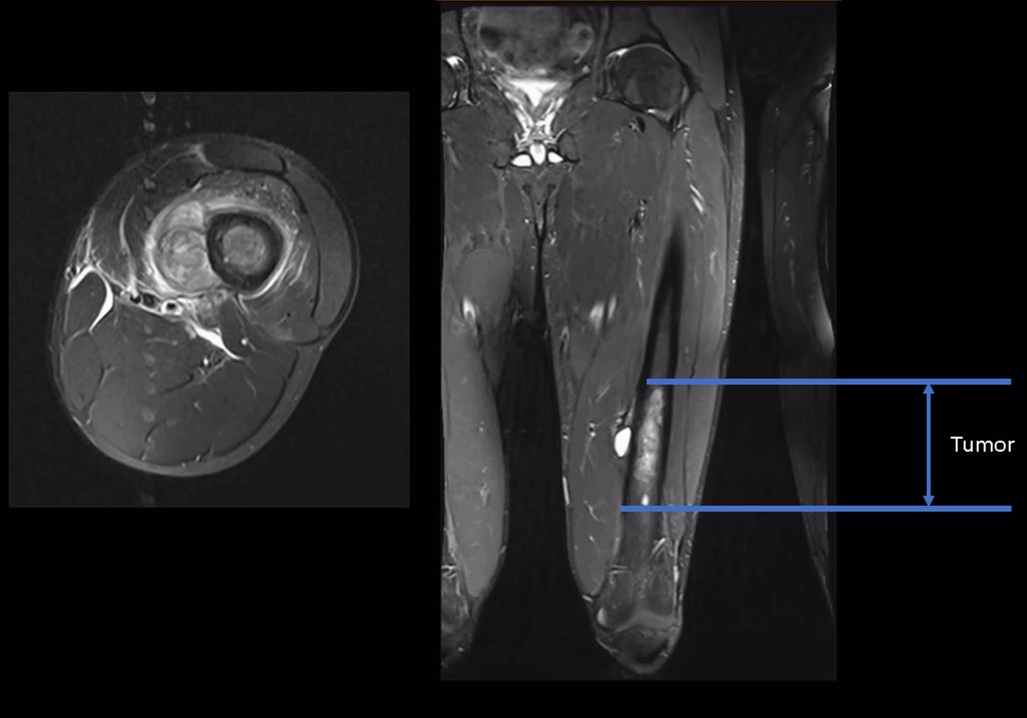
JBJS Deputy Editor for Social Media Dr. Matt Schmitz offers this post on a new study that evaluates peroneal nerve decompression and proximal fibular osteochondroma
Category: Oncology
Recent findings in orthopaedic oncology and musculoskeletal tumor management are highlighted in the new JBJS Guest Editorial What’s New in Musculoskeletal Tumor Surgery. Here, we

Recent findings related to bone loss and bone healing, among other important topics, are presented in the new JBJS Guest Editorial What’s New in Musculoskeletal

An international team of musculoskeletal oncology experts have explored several important questions regarding the surgical treatment of patients through secondary analyses of data from the
Recent studies on therapies for soft-tissue tumors, prophylactic antibiotic regimens, and other key topics are presented in the new JBJS Guest Editorial “What’s New in
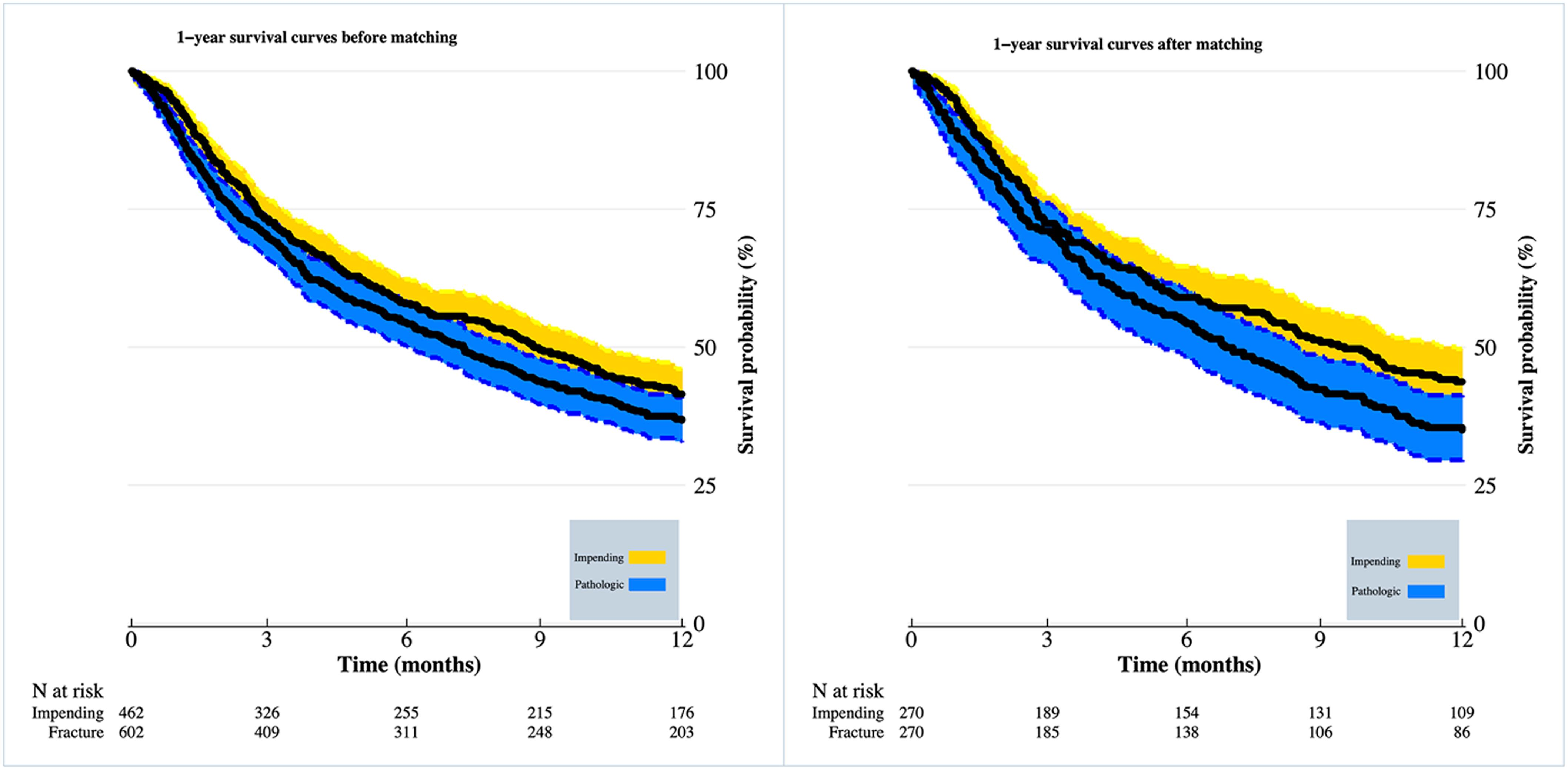
When patients present with identified bone metastases, a known primary diagnosis, and pain, the orthopaedic surgeon is nearly always contacted. The treatment plan is guided
Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, author
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a
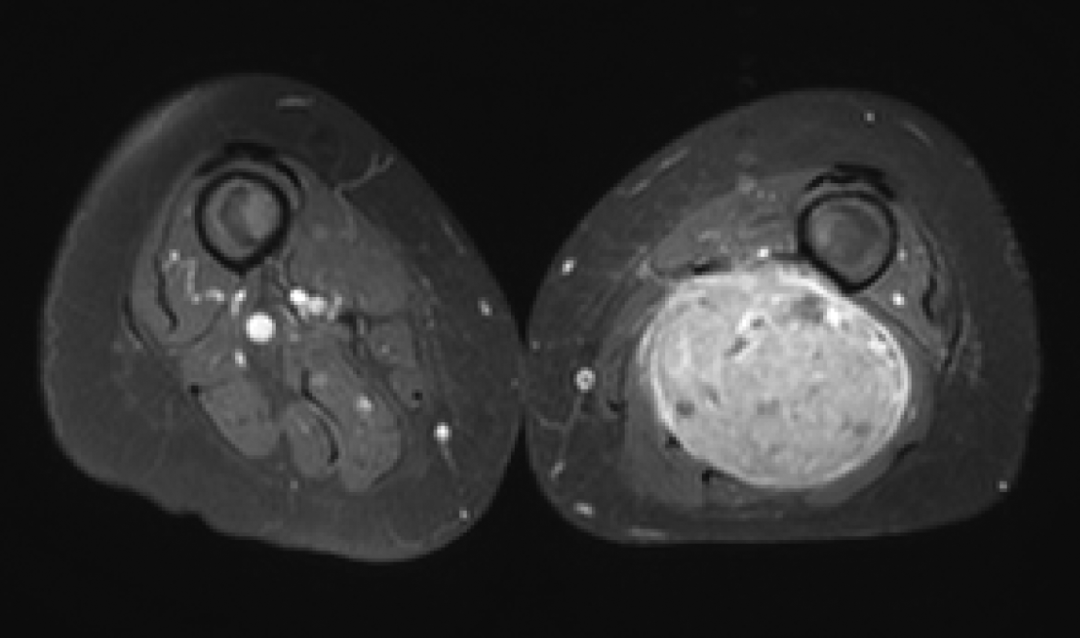
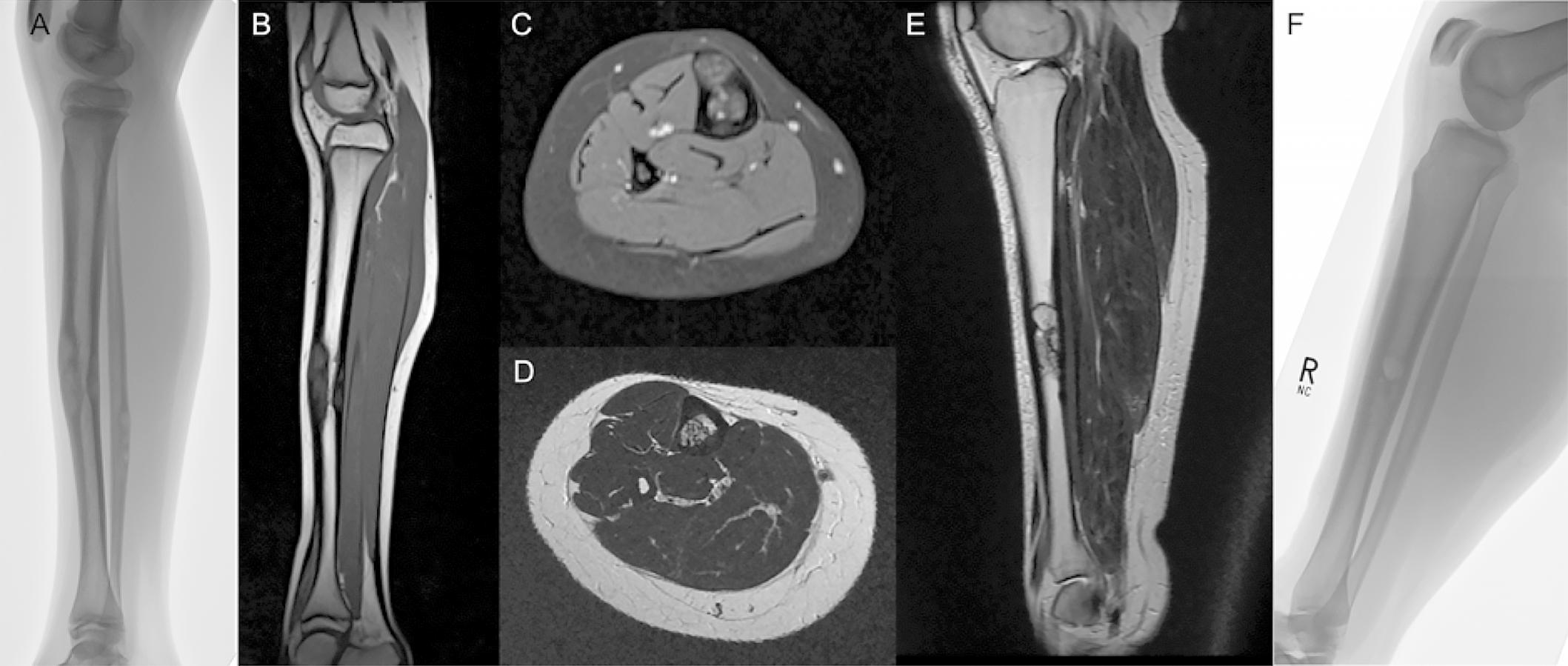
The international multicenter study by Schutgens et al. in the October 7, 2020 issue of JBJS reports findings from an analysis of >300 cases of
Tumor resections from the pelvic girdle often pose daunting reconstruction challenges for orthopaedic surgeons. In the September 2, 2020 issue of The Journal of Bone