Topics of interest in orthopaedic rehabilitation, including platelet-rich plasma injections and novel minimally invasive techniques, are presented in the new JBJS Guest Editorial What’s New
Category: Elbow
Recent findings in shoulder and elbow surgery are highlighted in the new JBJS Guest Editorial What’s New in Shoulder and Elbow Surgery. Here, we summarize

Noteworthy findings regarding topics such as platelet-rich plasma injection, botulinum toxin injection, and microinvasive trigger-finger release, among others, are presented in the new JBJS Guest
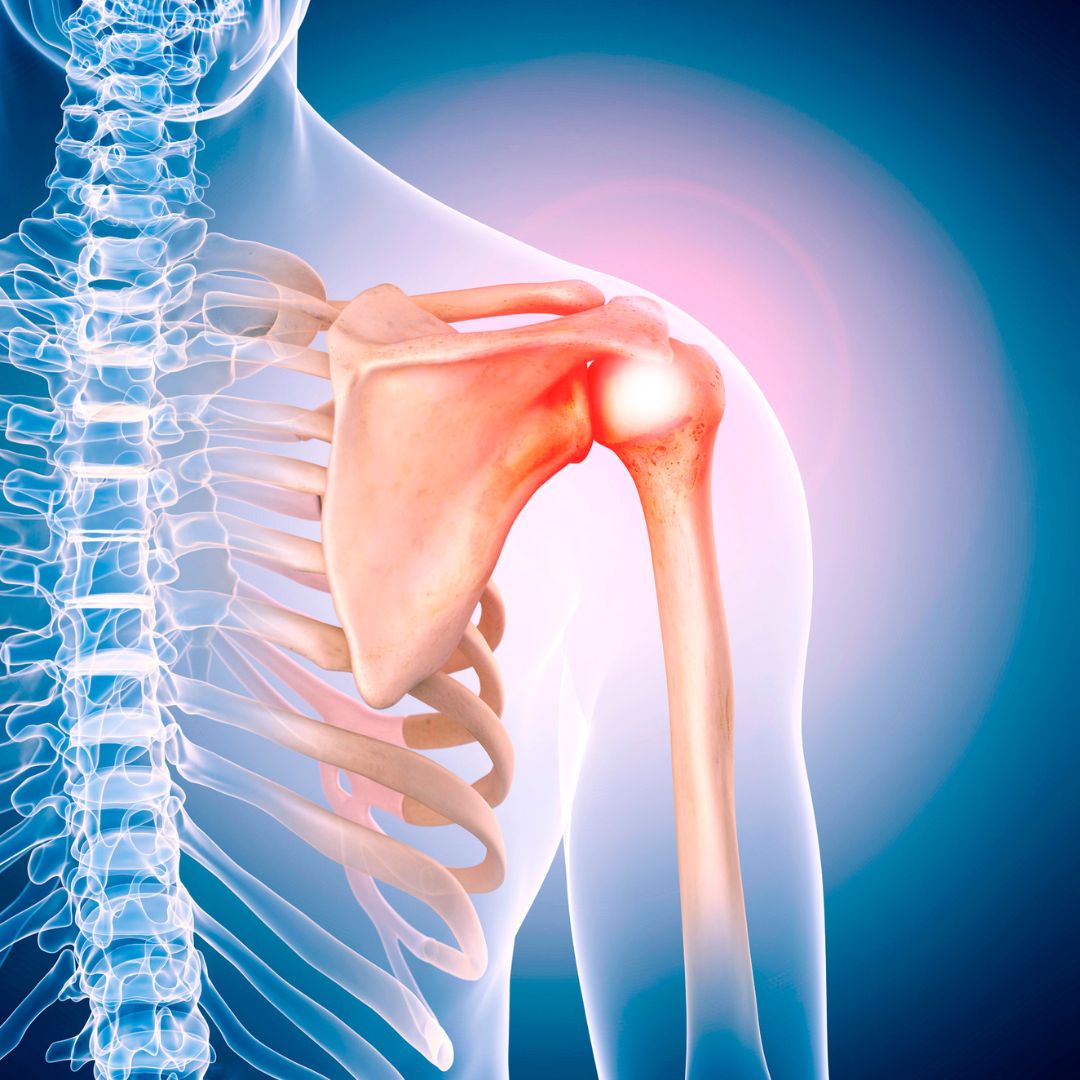
Recent findings in rotator cuff repair, shoulder arthroplasty, and fracture management are among the topics of interest in the new JBJS Guest Editorial What’s New
Botulinum toxin treatment of plantar fasciitis, clinical applications of point-of-care ultrasound, and other key topics are presented in the new JBJS Guest Editorial “What’s New
Rotator cuff repair, shoulder arthroplasty, shoulder instability, and the treatment of elbow injuries are among the topics of recent studies reviewed in the new JBJS
Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. Click here for a collection of all such OrthoBuzz Guest Editorial summaries.
In the May 5, 2021 issue of JBJS, Tomizuka et al. report the results of mechanical testing in which they quantified the loss of supination
Lower-extremity joint replacement is quite well-advanced, thanks to a high incidence of disabling osteoarthritis and a 40-plus-year history of development in hip and knee prostheses.
Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties. Click here for a