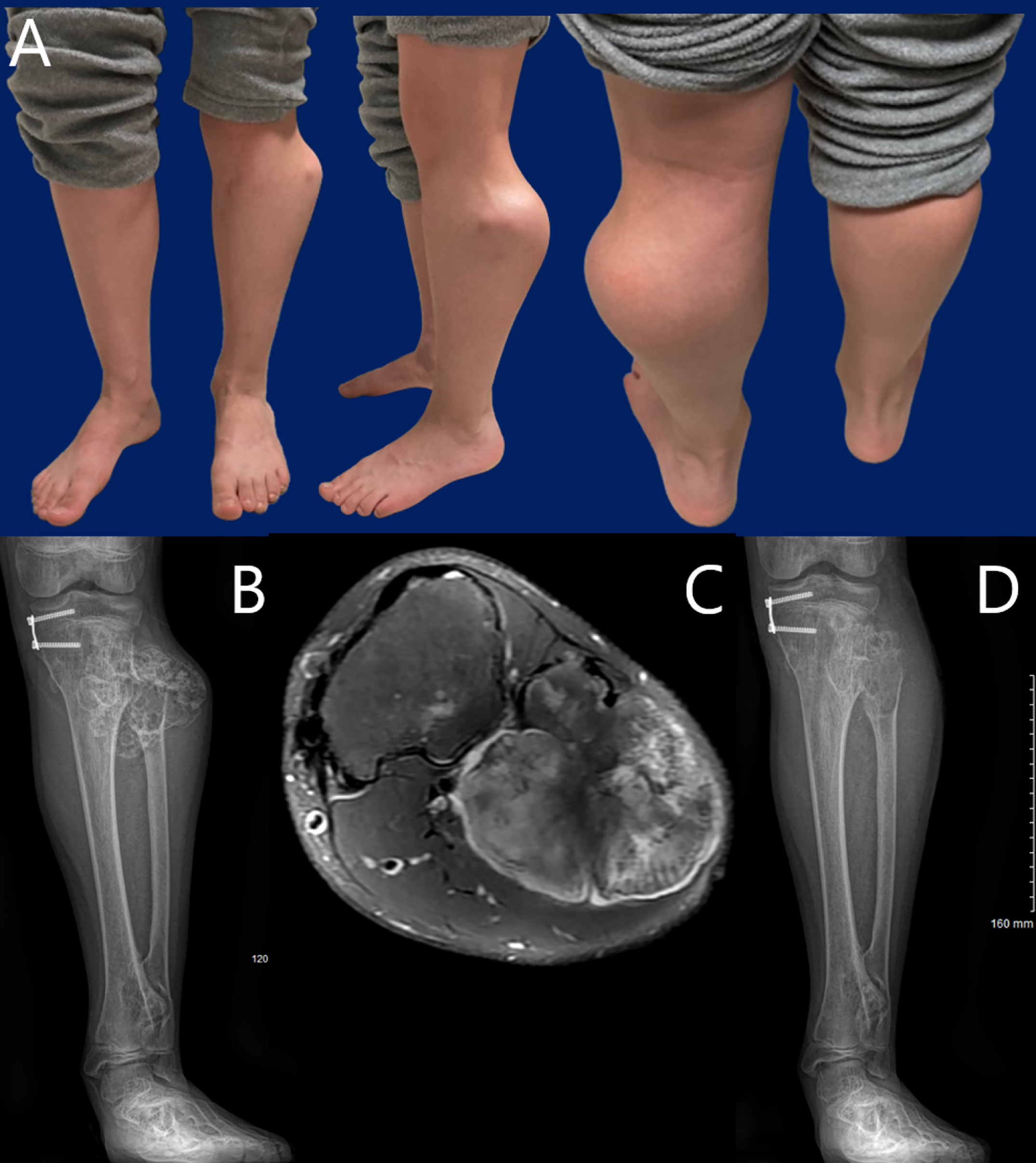
JBJS Deputy Editor for Social Media Dr. Matt Schmitz offers this post on a new study that evaluates peroneal nerve decompression and proximal fibular osteochondroma
Category: Pediatrics

In this post, Deputy Editor for Social Media Matt Schmitz discusses a study by Sato et al. now available in JBJS. Developmental dysplasia of the
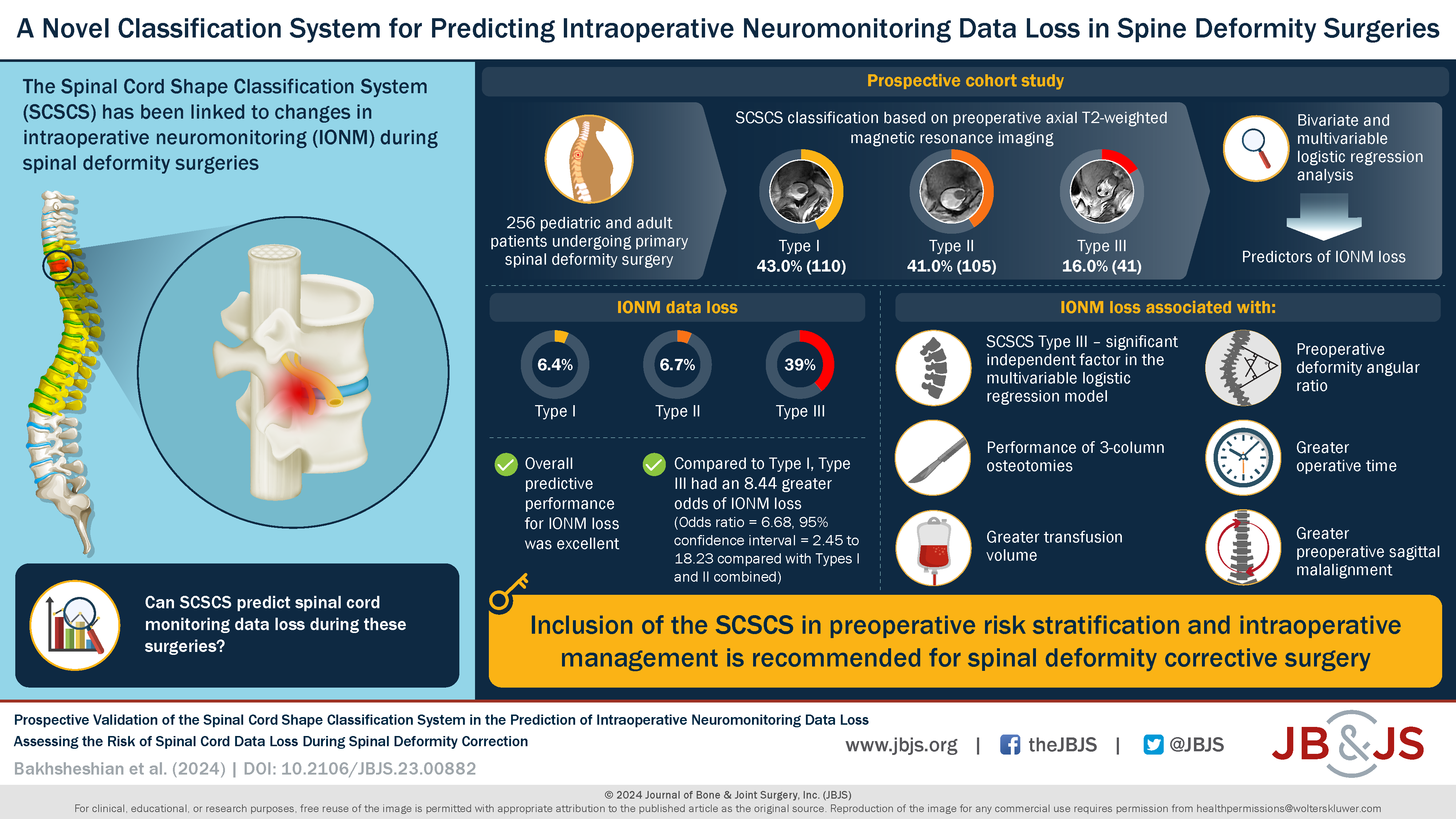
In a study now published in JBJS, Bakhsheshian et al. sought to prospectively validate use of the Spinal Cord Shape Classification System (SCSCS) to identify
A video abstract is available with the new study by Chan et al. in JBJS: A Rapid MRI Protocol for the Evaluation of Acute Pediatric Musculoskeletal
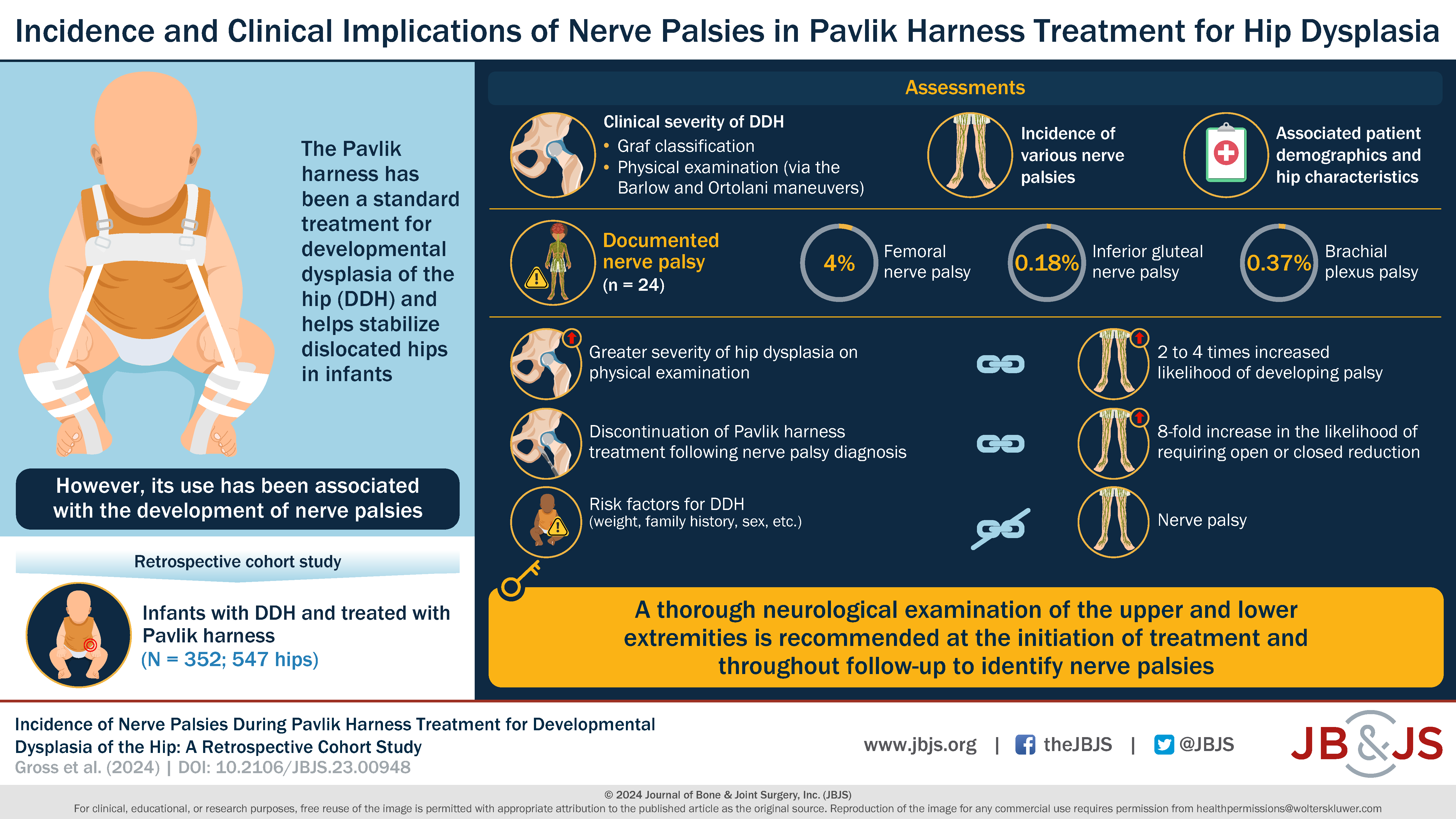
What is the incidence of nerve palsy in infants undergoing Pavlik harness treatment for developmental dysplasia of the hip (DDH)? Dr. Matt Schmitz, JBJS Deputy
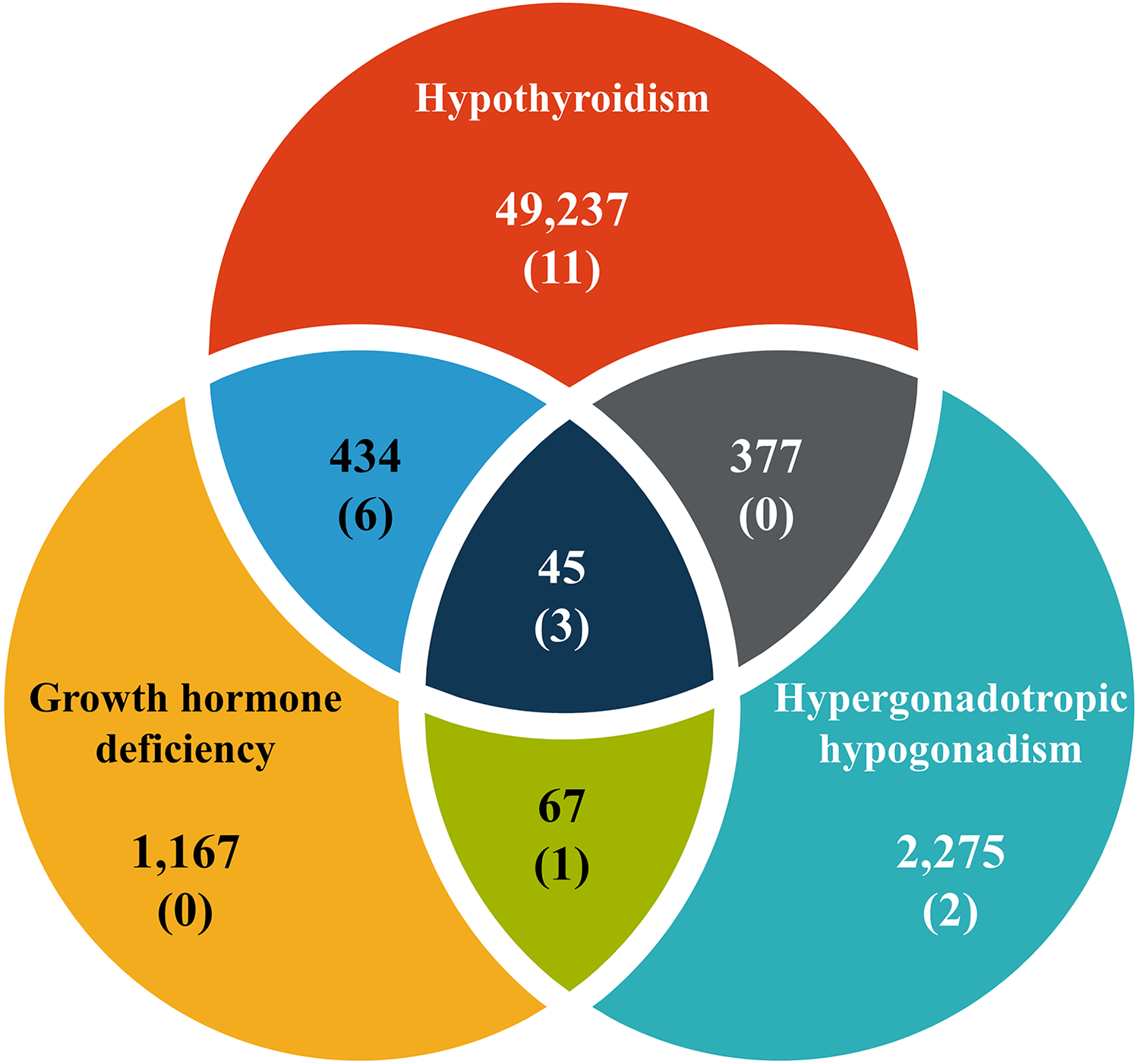
Endocrinopathy has been identified as a risk factor for slipped capital femoral epiphysis (SCFE). In young patients with endocrinopathy, what is the incidence of SCFE?
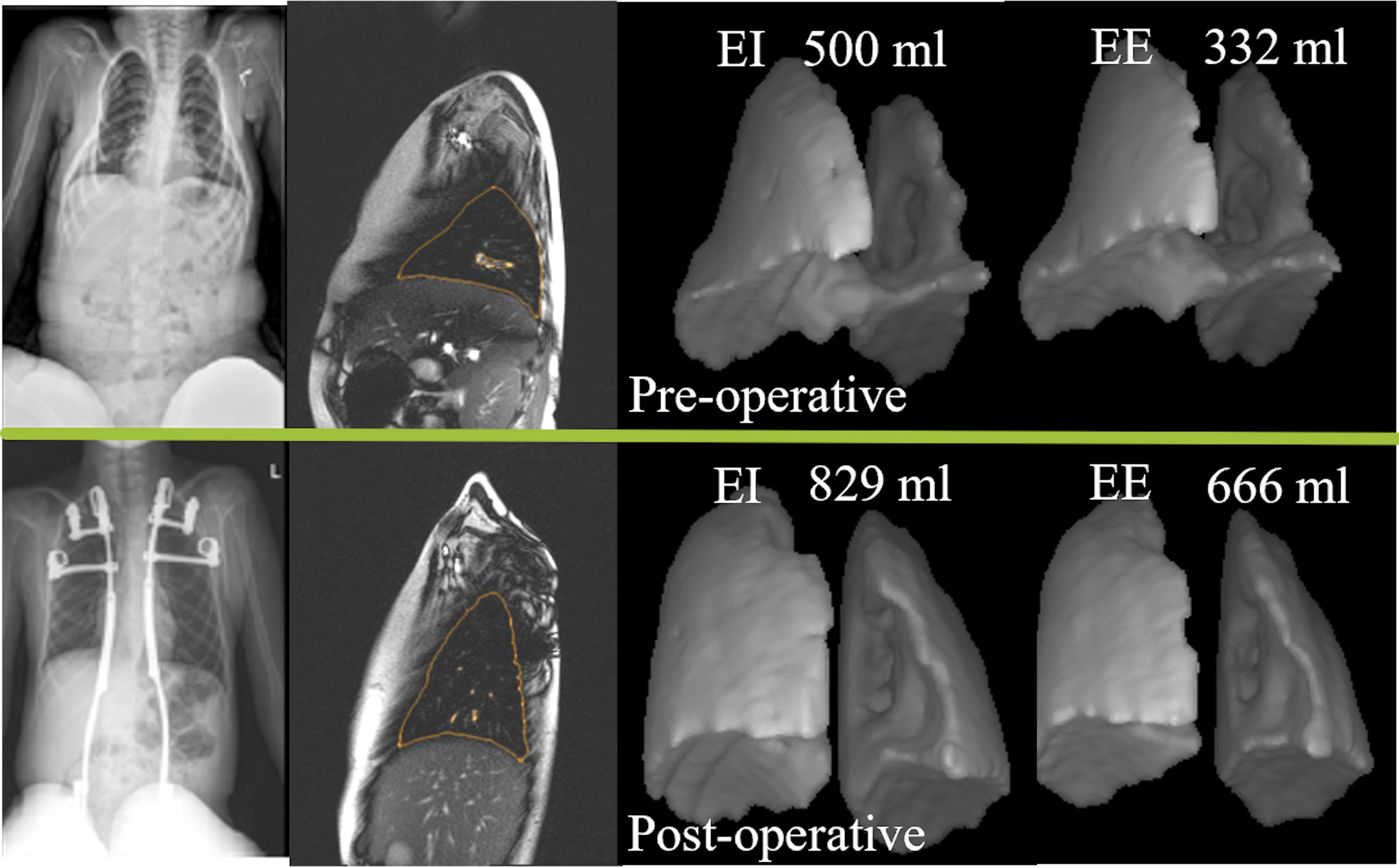
Notable findings in pediatrics regarding the treatment of fractures, infection, early-onset scoliosis, and more are presented in the new JBJS Guest Editorial What’s New in
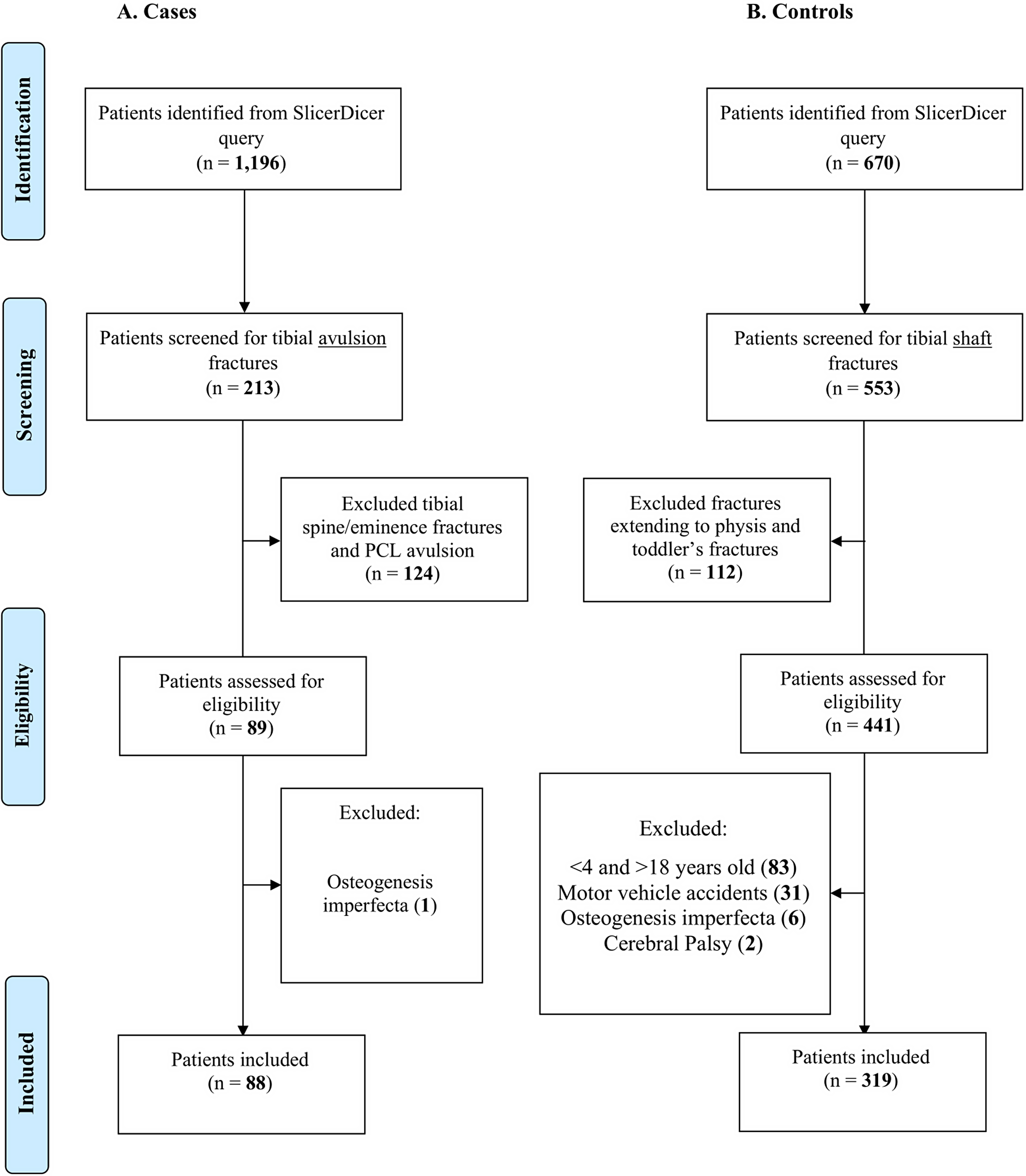
Dr. Matt Schmitz, JBJS Deputy Editor for Social Media, offers this post on a new study that explores whether a greater proportion of pediatric patients
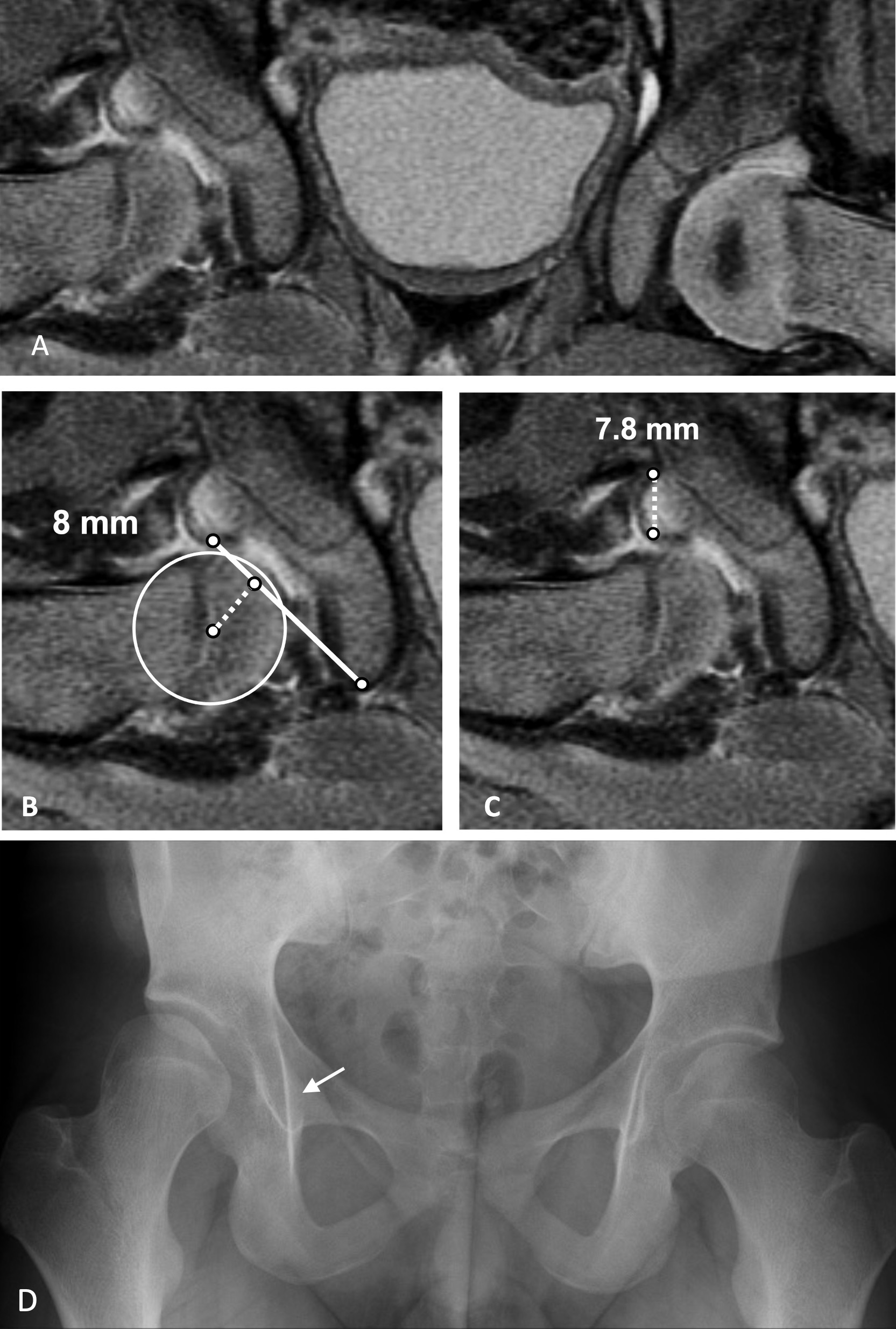
JBJS Deputy Editor for Social Media Dr. Matt Schmitz discusses a new study assessing the use of post-reduction MRI measurements to help predict residual acetabular
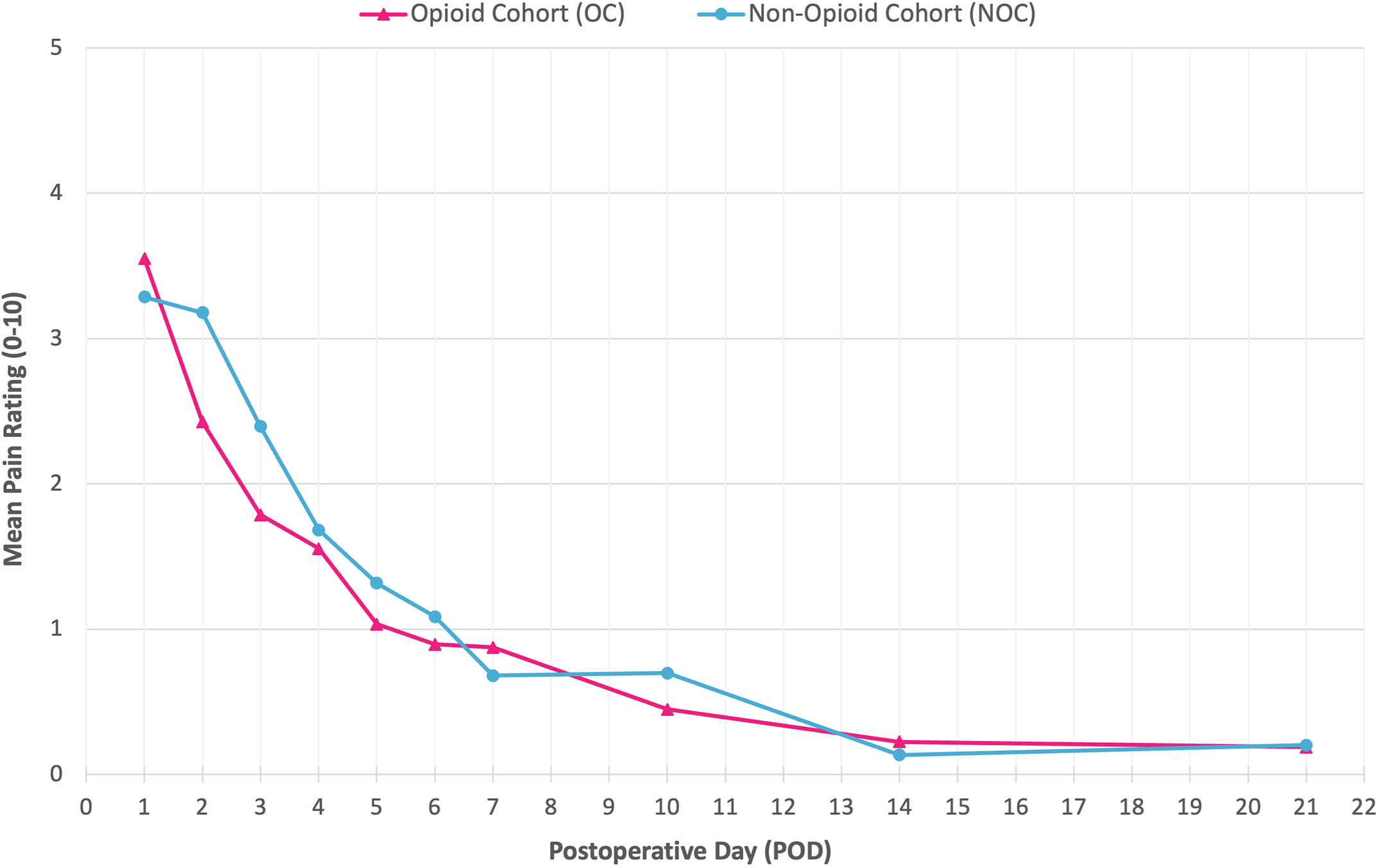
JBJS Deputy Editor for Social Media Dr. Matt Schmitz offers his thoughts on a new study comparing the efficacy of opioid and non-opioid analgesia following