Key findings related to the prevention and treatment of periprosthetic joint infection (PJI), among other important topics, are presented in the new JBJS Guest Editorial
Category: What’s New
Topics of interest in orthopaedic trauma, including fracture fixation, pain management, and more, are highlighted in the new JBJS Guest Editorial What’s New in Orthopaedic

Recent findings in spine surgery on topics such as lumbar facet arthroplasty, pain management, nicotine use, and more are presented in the new JBJS Guest

Topics of interest in foot and ankle surgery, including hallux valgus recurrence, simultaneous vs. sequential total ankle arthroplasty (TAA), and more, are featured in the

Key findings in sports medicine on topics such as rotator cuff repair, anterior cruciate ligament (ACL) reconstruction, and more are presented in the new JBJS
Nonoperative treatment outcomes, the efficacy of waterproof cast protectors, and other topics of interest are presented in the new JBJS Guest Editorial What’s New in
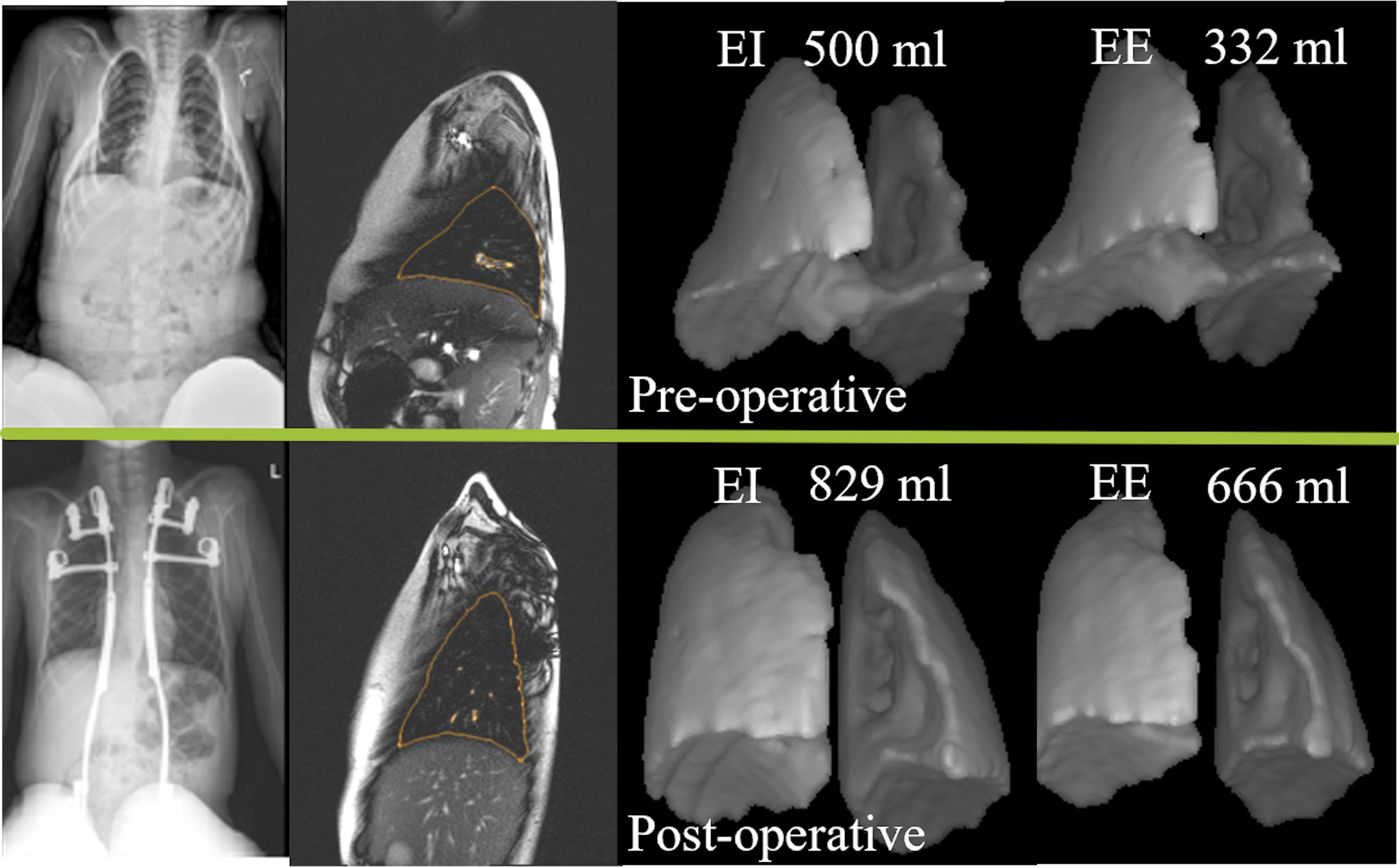
Notable findings in pediatrics regarding the treatment of fractures, infection, early-onset scoliosis, and more are presented in the new JBJS Guest Editorial What’s New in

Findings from high-level and award-winning studies on topics such as unicompartmental and total knee arthroplasty (TKA), among others, are featured in the new JBJS Guest
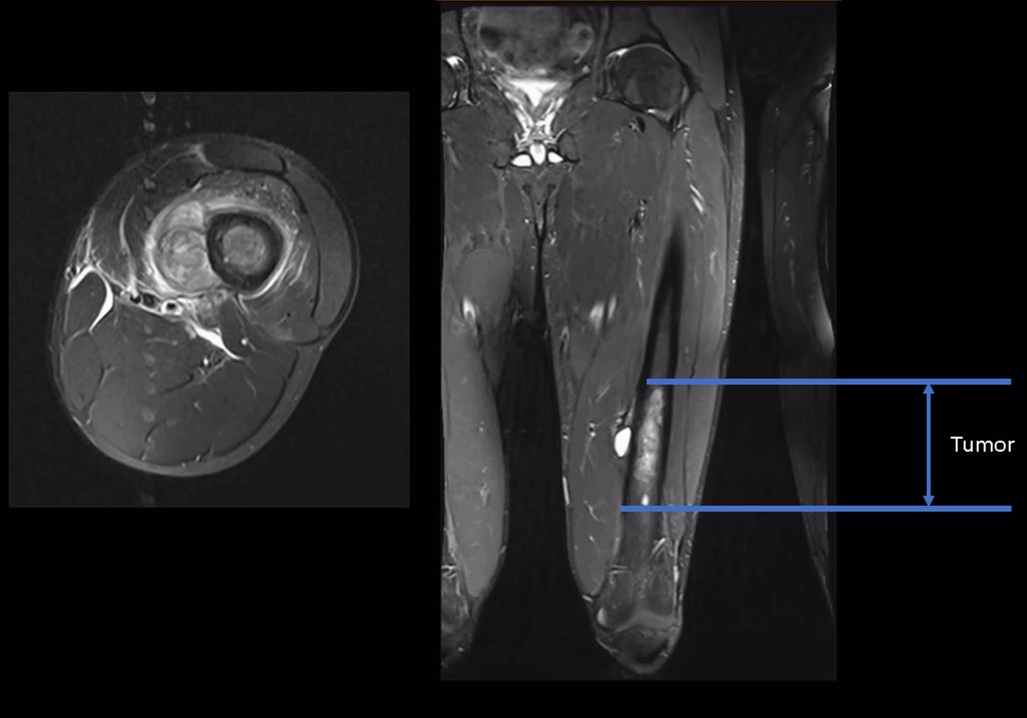
Recent findings in orthopaedic oncology and musculoskeletal tumor management are highlighted in the new JBJS Guest Editorial What’s New in Musculoskeletal Tumor Surgery. Here, we

Recent findings related to bone loss and bone healing, among other important topics, are presented in the new JBJS Guest Editorial What’s New in Musculoskeletal