Key findings in sports medicine on topics such as rotator cuff repair, anterior cruciate ligament (ACL) reconstruction, and more are presented in the new JBJS
Category: Shoulder
Recent findings in rotator cuff repair, shoulder arthroplasty, and fracture management are among the topics of interest in the new JBJS Guest Editorial What’s New
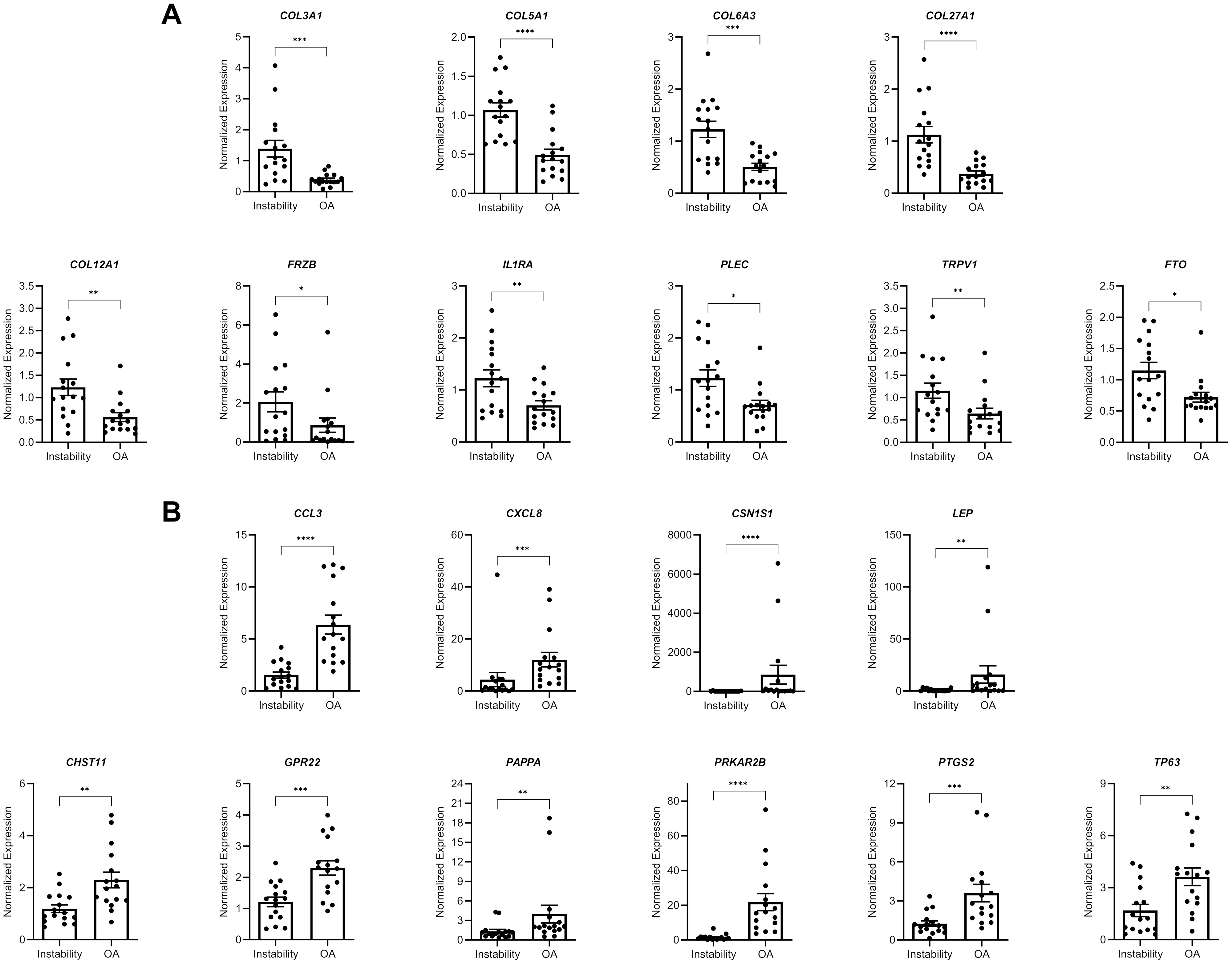
A new JBJS study presents novel data on gene expression in glenoid cartilage following shoulder instability. JBJS Deputy Editor for Social Media Dr. Matt Schmitz

Recent reports in JBJS Case Connector describe 2 orthopaedic cases involving the formation of “rice bodies,” fibrinous loose bodies with a rice-like appearance. As discussed

Topics of interest in the new JBJS Guest Editorial “What’s New in Sports Medicine” include opioid-sparing analgesia, risk of graft failure following meniscal allograft transplantation,
Rotator cuff repair, shoulder arthroplasty, shoulder instability, and the treatment of elbow injuries are among the topics of recent studies reviewed in the new JBJS

Co-author Rachel M. Frank, MD summarizes the 5 most compelling findings from among the studies highlighted in the new “What’s New in Sports Medicine” in JBJS.

This OrthoBuzz guest post comes from Paul E. Matuszewski, MD, in response to a recent article in the New York Times. The ever-increasing importance of
Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. Click here for a collection of all such OrthoBuzz Guest Editorial summaries.
Patient surveys are now being widely used by hospital systems to monitor patient satisfaction with the process of inpatient and outpatient musculoskeletal care. While data from the surveys can help guide

