Topics of interest in foot and ankle surgery, including hallux valgus recurrence, simultaneous vs. sequential total ankle arthroplasty (TAA), and more, are featured in the
Category: Foot and Ankle
Editor-in-Chief Dr. Marc Swiontkowski discusses a new study in JBJS examining the effect of age on complication rates and patient-reported outcomes after total ankle arthroplasty
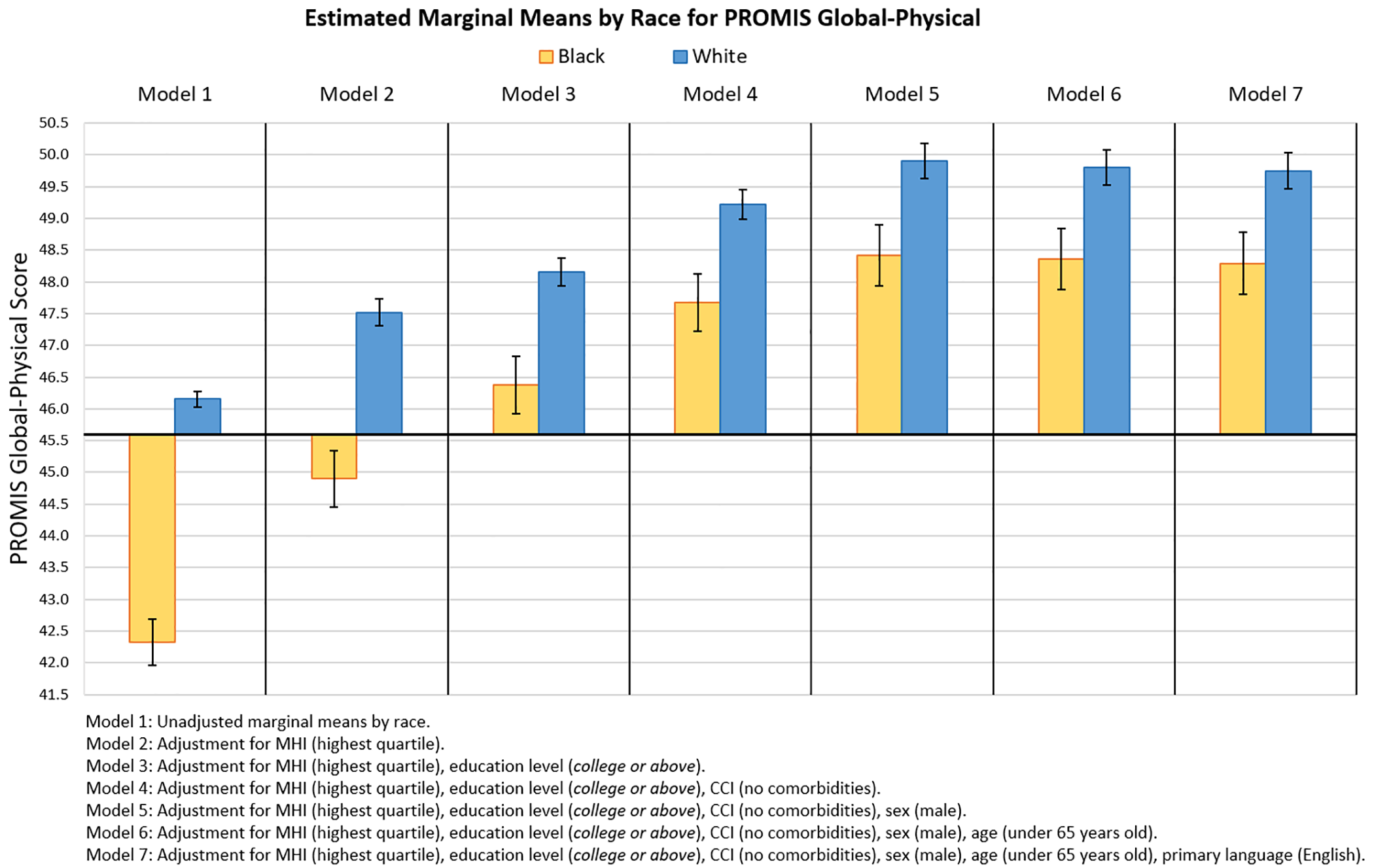
A new study evaluates sociodemographic factors impacting racial and ethnic disparities in baseline PROM scores of foot and ankle patients. JBJS Editor-in-Chief Dr. Marc Swiontkowski

Long-term survivorship of total ankle arthroplasty, rerupture rates associated with the treatment of acute Achilles tendon rupture, and other important findings are presented in the
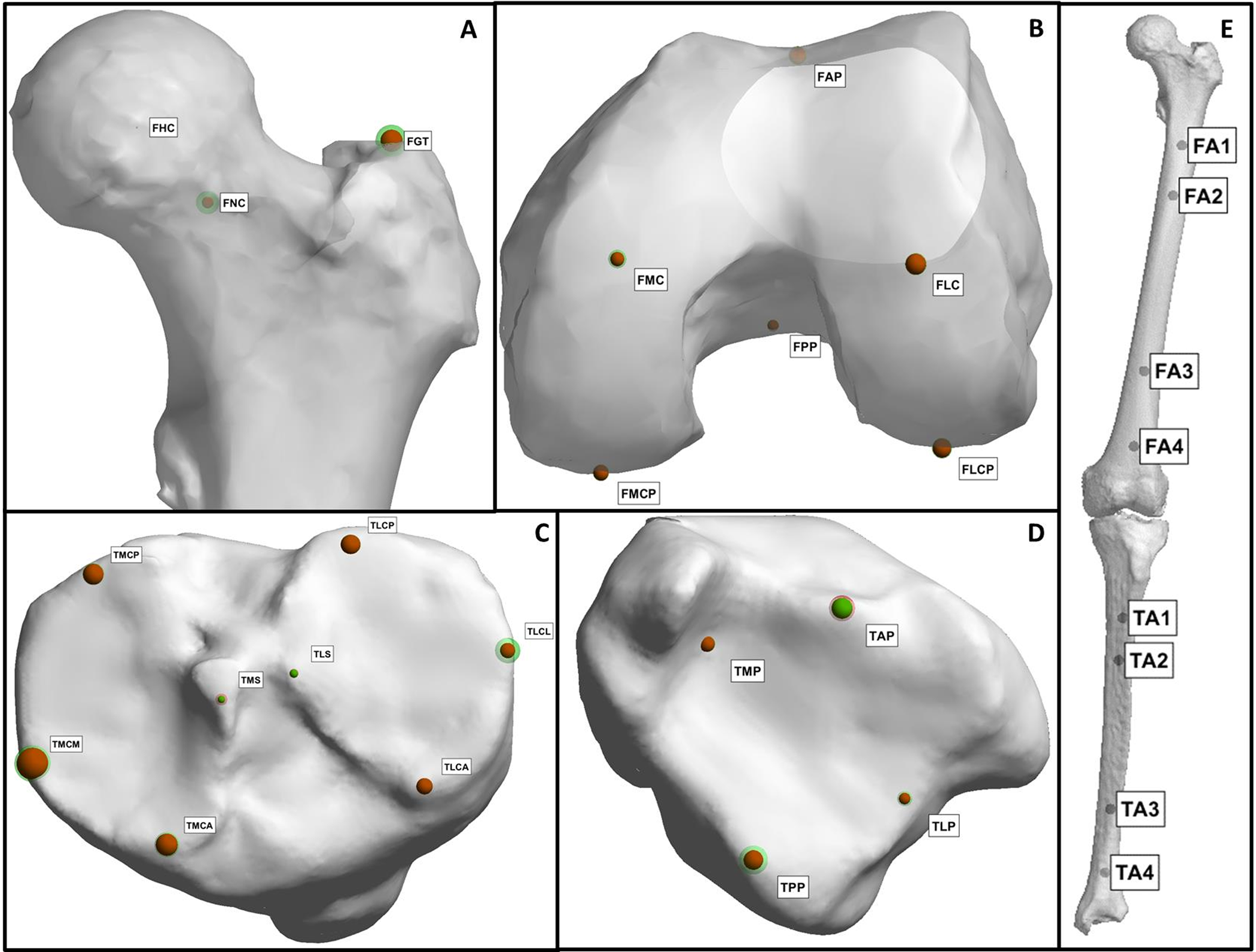
Editor-in-Chief Dr. Marc Swiontkowski discusses a new study from The Netherlands that presents a fully automatic method for assessing lower-limb alignment from computed tomography (CT)
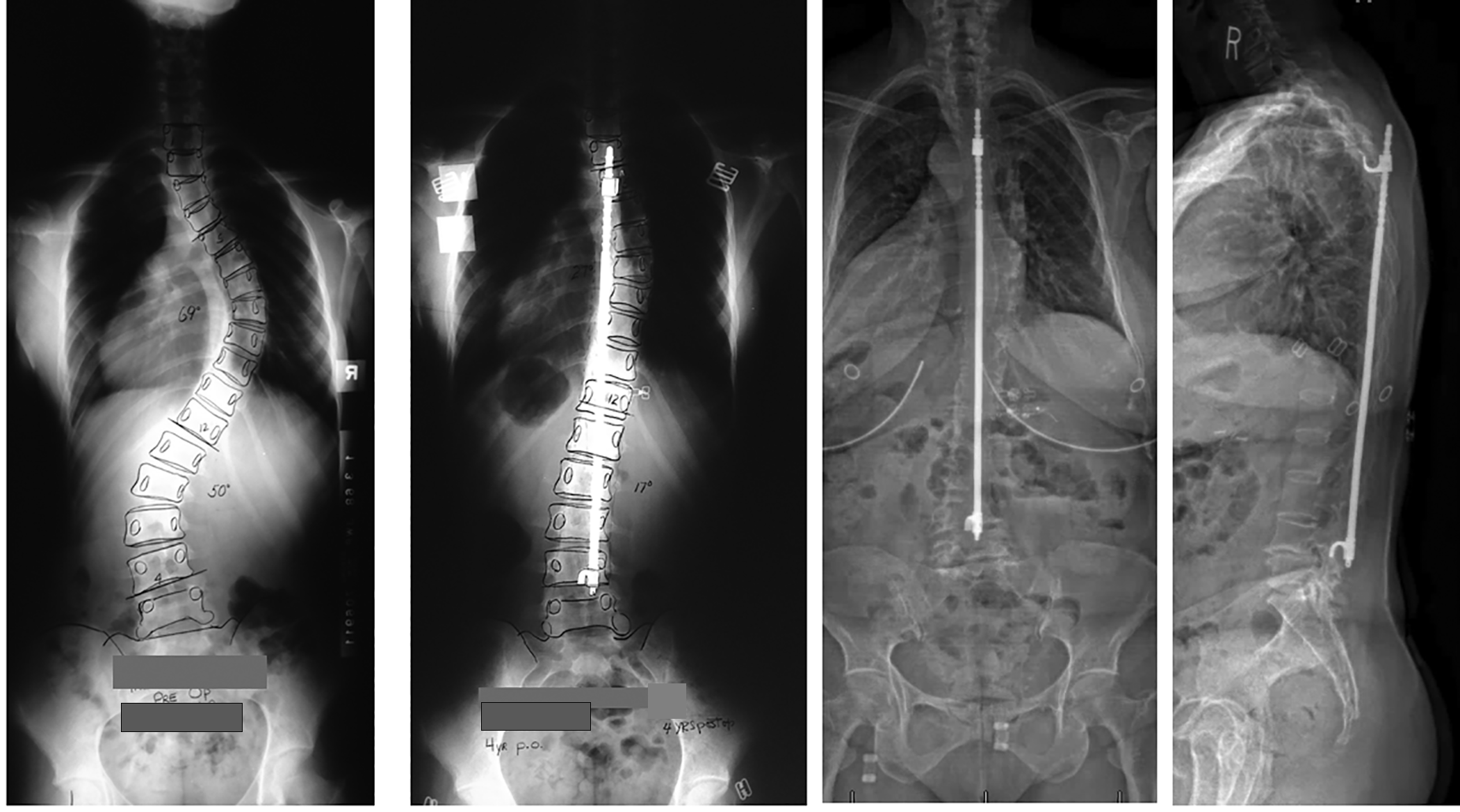
Patient outcomes ≥40 years after treatment for adolescent idiopathic scoliosis, return-to-sport rates following periacetabular osteotomy, and other important findings are covered in the new JBJS
Botulinum toxin treatment of plantar fasciitis, clinical applications of point-of-care ultrasound, and other key topics are presented in the new JBJS Guest Editorial “What’s New
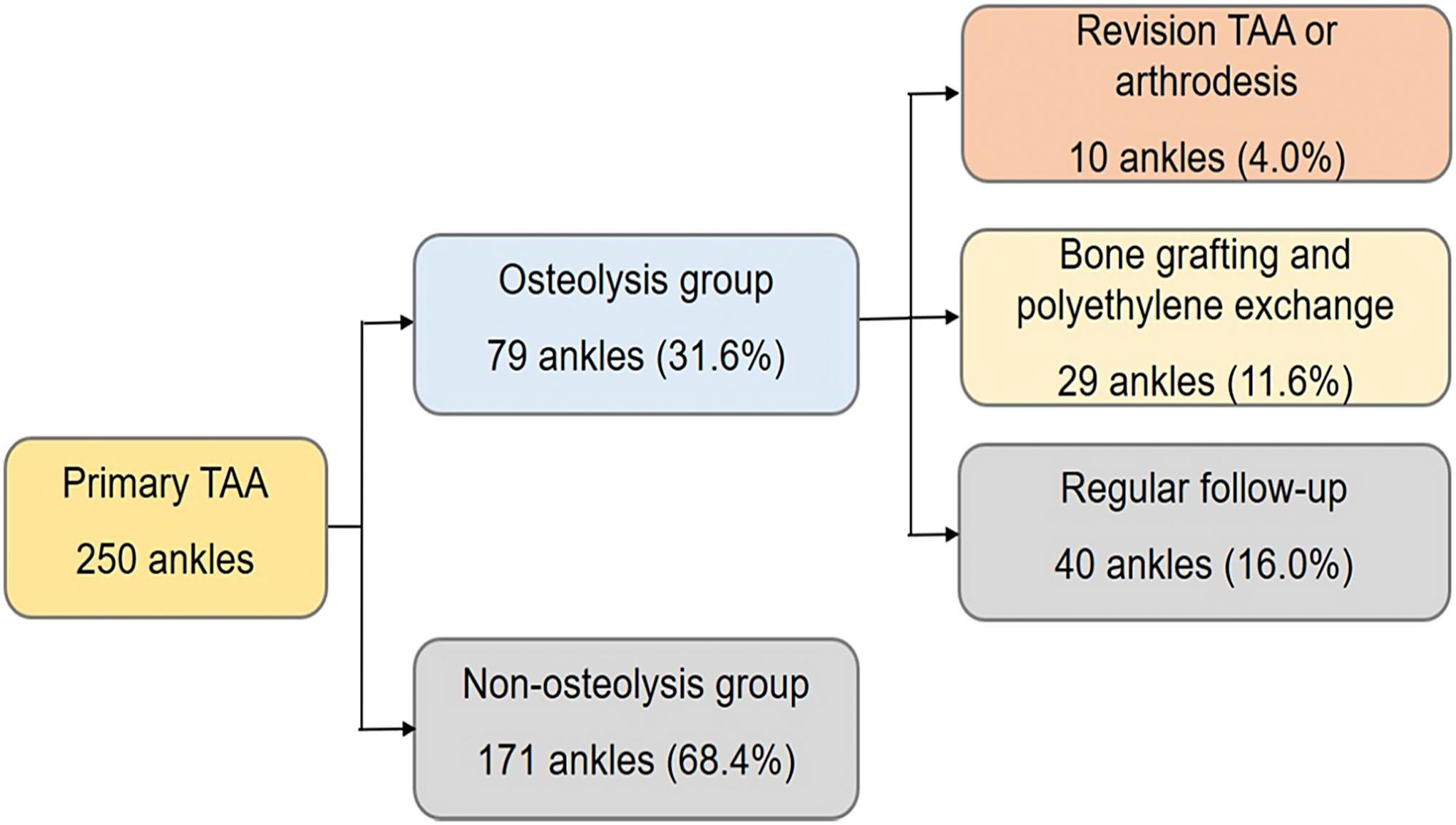
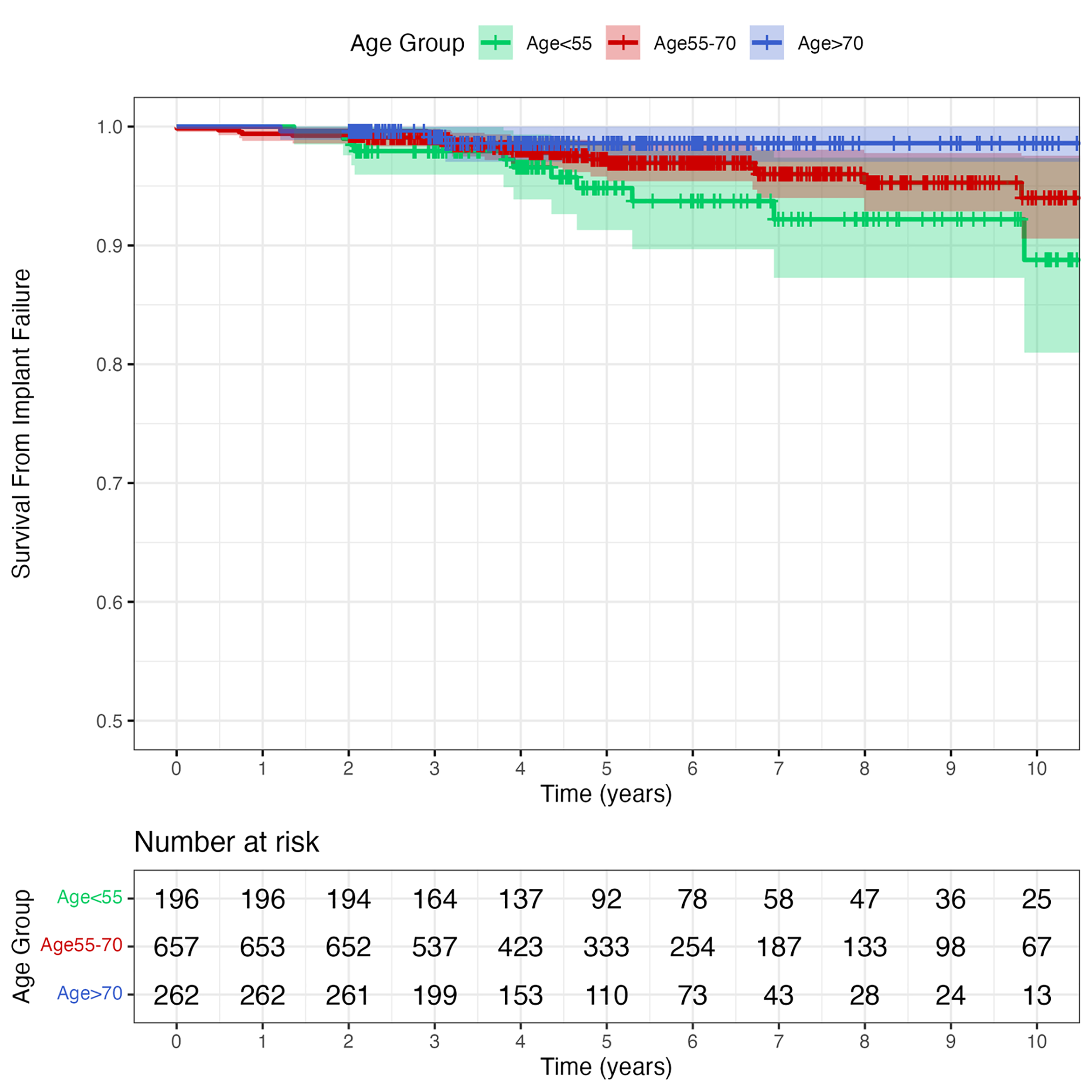
Total ankle arthroplasty (TAA) continues to gain favor as an alternative to ankle arthrodesis. However, periprosthetic osteolysis is a risk factor for a poor outcome.
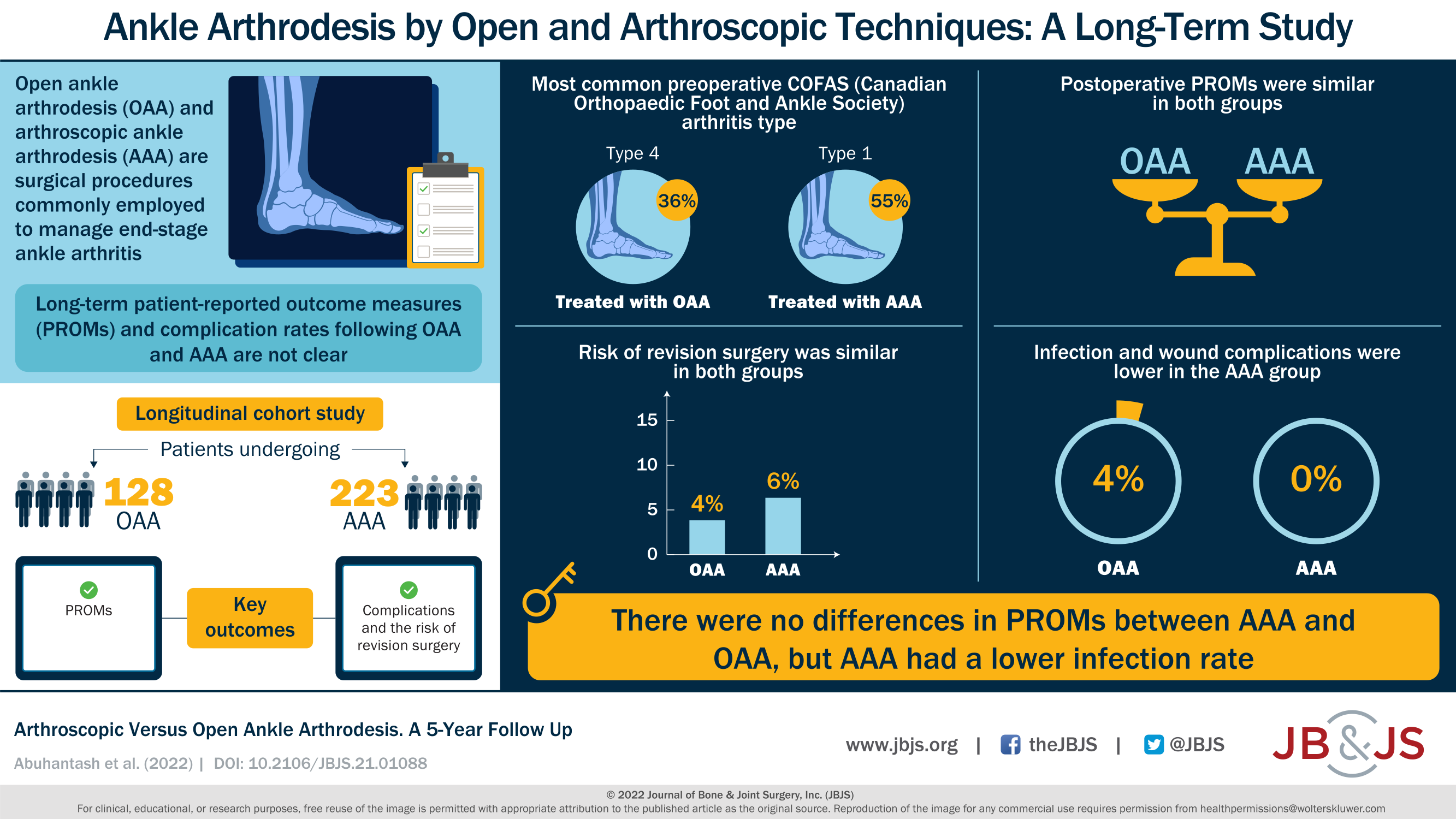
A new JBJS report compares arthroscopic versus open ankle arthrodesis. The authors analyzed long-term patient-reported outcomes, major complications, and reoperations. JBJS Editor-in-Chief Dr. Marc Swiontkowski

Co-author Walter C. Hembree, MD selects the 5 most compelling findings from the recently published “What’s New in Foot and Ankle Surgery.” Hallux Rigidus – A

