The findings of a new animal study suggest that bisphosphonate treatment in donors may indeed be relevant when mineralized allografts are used in orthopaedic procedures. Editor-in-Chief Dr. Marc Swiontkowski discusses this new JBJS report.
The worldwide orthopaedic community has been working over the last 2 decades to improve the diagnosis and treatment of osteoporosis in patients who present with a fragility fracture. These important efforts have met with some success. Among treatments, bisphosphonates are widely used in osteoporosis as well as for select other diseases to slow bone loss.
At the same time, allografts are an important adjunctive source in such areas as fracture management and revision arthroplasty. With growth in the use of bisphosphonates to limit the risk of secondary fractures related to osteoporosis, it’s likely that we may then see an increase in a history of bisphosphonate treatment in our donor populations.
What impact, if any, does bisphosphonate exposure have on the integration of bone allografts?
Study Overview
In the current issue of JBJS, Cohen et al. report their findings of a set of 2 animal studies. The researchers’ goal: to determine whether mineralized block allografts and allograft particles from donors treated with bisphosphonates have different properties vs. allografts from donors with no history of oral bisphosphonate treatment.
- Human block allografts from 3 donors treated with bisphosphonates and 3 age and sex-matched controls were used.
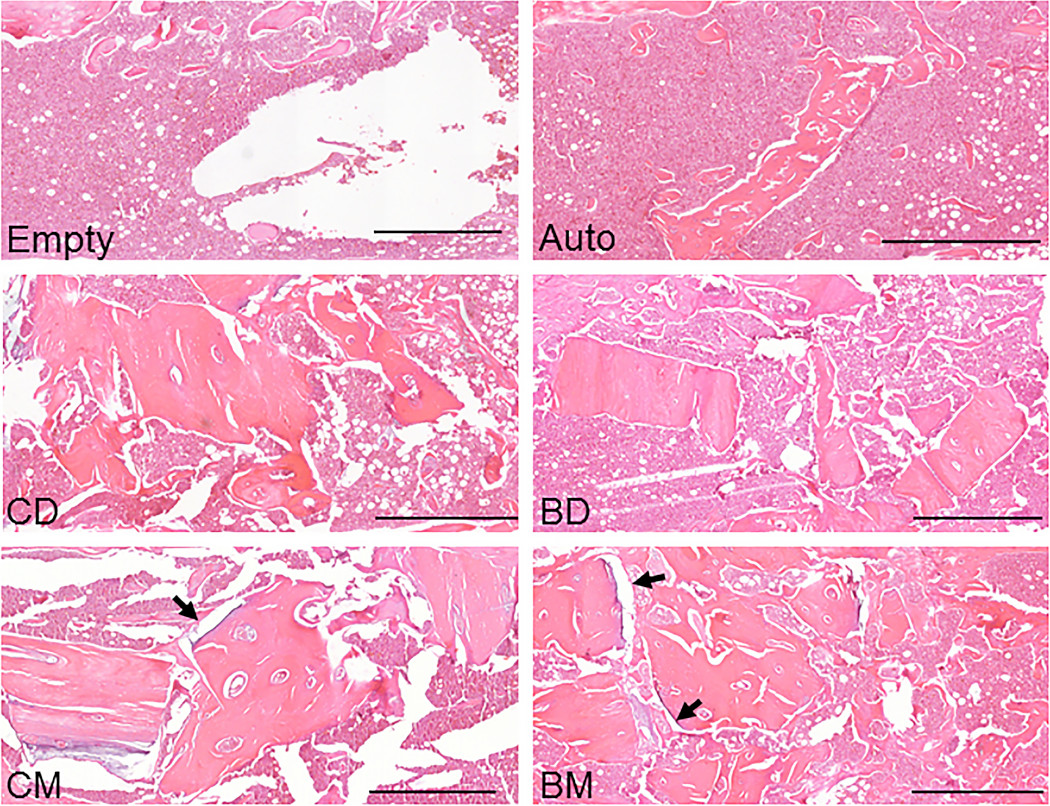
- In study #1, mineralized and demineralized cylindrical grafts were placed bilaterally in the femoral metaphysis of 56 rats.
- In study #2, pooled samples from each group were prepared as particles and implanted bilaterally in the femoral marrow canal of 24 rats.
- Osseointegration was evaluated at 10 weeks by micro-CT and histomorphometry.
Study Findings
The researchers found that mineralized allografts were osseointegrated but were not remodeled or replaced by living bone. Of particular note, they found that bisphosphonate exposure impacted osteogenesis, preventing osseointegration and remodeling.
The findings are highly relevant to the clinical use of allograft bone. In the study, sites treated with demineralized samples had greater bone volume, which may reinforce the known notion that demineralization is one important component of allograft bone management. In terms of mineralized allografts, I agree with the authors that the use of those with bisphosphonate exposure warrants further evaluation. Routine tracking of donor medications with the potential disqualifier of prior bisphosphonate use may be an appropriate next step—while we remain committed to efforts to reduce fragility fractures with all appropriate treatments.
Access the full report by Cohen et al., including a downloadable infographic.
Marc Swiontkowski, MD
JBJS Editor-in-Chief
Related reading on OrthoBuzz: “What’s New in Osteoporosis and Fragility Fractures 2022,” “The Cost-Effectiveness of Fragility-Fracture Screening and Prevention”