Editor-in-Chief Dr. Marc Swiontkowski reflects on a new study that examines the capture of patient-reported outcome measures (PROMs) after total joint arthroplasty. He offers a suggestion toward reducing the rate of follow-up loss.
Orthopaedic surgery has been at the forefront of understanding the importance of patient-reported outcome measures (PROMs) for over 20 years. In the 1990s, the American Academy of Orthopaedic Surgeons (AAOS) established an outcomes committee, with leadership guidance of individuals such as Dr. Robert Keller and Dr. Clem Sledge. The effort was informed by the seminal work of Dr. Jack Wennberg from Dartmouth in the field of small-area analysis, which detailed the high degree of regionality in the use of surgical procedures1. Regionality was thought to be a result of training-program influence as well as local “custom.” One answer to address this regional variation was to better understand patient preferences and outcomes for various procedures. The outcomes committee worked hard to develop and validate PROMs and make the AAOS membership aware of their power through the AAOS MODEMs (Musculoskeletal Outcomes Data Evaluation and Management System) program.
Fast forward 2+ decades and PROMs are widely used and accepted as research tools to help identify procedures with the optimum patient benefit. We have now entered an era in which payors are requiring the collection and reporting of PROMs data. Obtaining pre-surgical PROMs data is fairly straightforward, with collection occurring at the office consultation visit. The collection of follow-up data, however, is the difficult part.
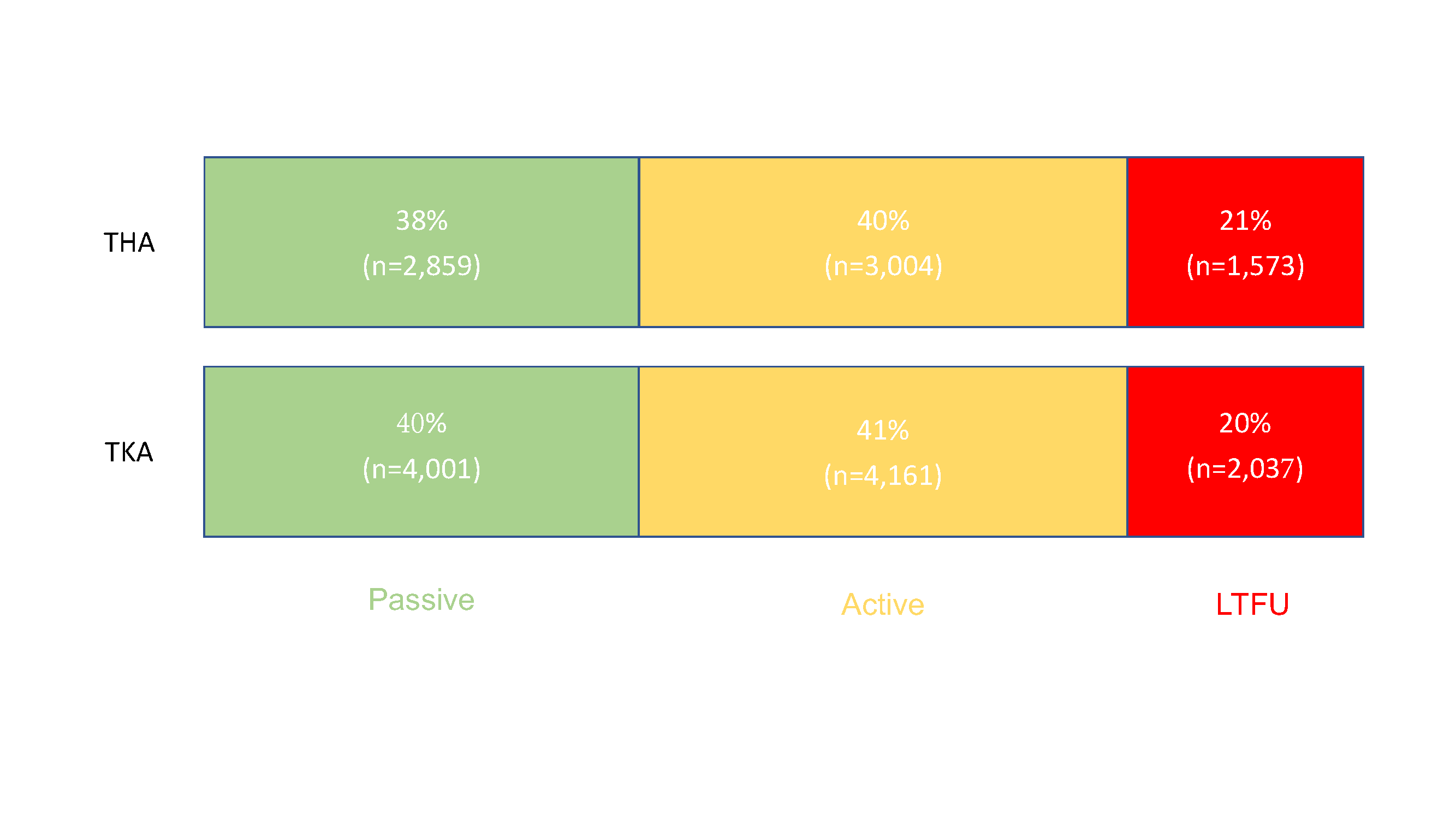
In the May 15, 2024 issue of JBJS, Rullán et al. report on their evaluation of active (staff-initiated) vs. passive (automated) methods of PROMs collection in a large arthroplasty practice at the Cleveland Clinic. They report that automated systems, while practical and cost-effective, fall short of adequately capturing PROMs data following total joint arthroplasty when used alone. Moreover, in the study, 21% of total hip and 20% of total knee arthroplasty patients were lost to follow-up. The study can be accessed at JBJS.org:
This prospective cohort study included more than 17,000 patients undergoing primary elective total hip arthroplasty (THA) or total knee arthroplasty (TKA) between January 2016 and December 2020. In the THA cohort, passive methods of collecting PROMs data were successful for 38%, while active measures were successful for 40%. In the TKA cohort, the corresponding percentages were 40% and 41%.
Overall, the authors found that 1 in 5 patients were lost to follow-up, despite whether active or passive data-collection methods were used. In addition, they found that the patients lost to follow-up were more likely to be younger, be male, be of Black or another non-White race, have fewer years of education, smoke, have Medicaid insurance, and have specific baseline PROM phenotypes (based on scores for pain, function, and/or mental health). Furthermore, they found that older age, Black race, and residing in areas of higher socioeconomic disadvantage were associated with higher odds of requiring active follow-up. In their discussion, the authors touch on several efforts that could improve follow-up and note the need for innovative strategies to enhance follow-up in diverse at-risk populations.
From my own decades of work in patient outcomes research, I would add that a missing element in the effort to improve data collection may be the surgeon. Having a patient’s own surgeon, whom they generally are appreciative of, request that the patient complete the PROM when it comes to them via email, mail, or text will most certainly result in lower “loss to follow-up.” It is with this relatively simple and quick intervention that response rates may increase, not only to satisfy insurer requirements but also to get a better understanding of patient functional outcomes following these procedures.
Read the full study: How to Raise the Bar in the Capture of Patient-Reported Outcome Measures in Total Joint Arthroplasty: Results from Active and Passive Follow-up Measures
JBJS Editor-in-Chief
References
- Swiontkowski MF, Buckwalter JA, Keller RB, Haralson R. The outcomes movement in orthopaedic surgery: where we are and where we should go. J Bone Joint Surg Am. 1999 May;81(5):732-40.