When patients present with identified bone metastases, a known primary diagnosis, and pain, the orthopaedic surgeon is nearly always contacted. The treatment plan is guided
Tag: metastasis
With the increasing effectiveness of immunotherapy and chemotherapy, patients with metastatic disease are surviving longer in much higher numbers. For many primary tumors (lung, breast,
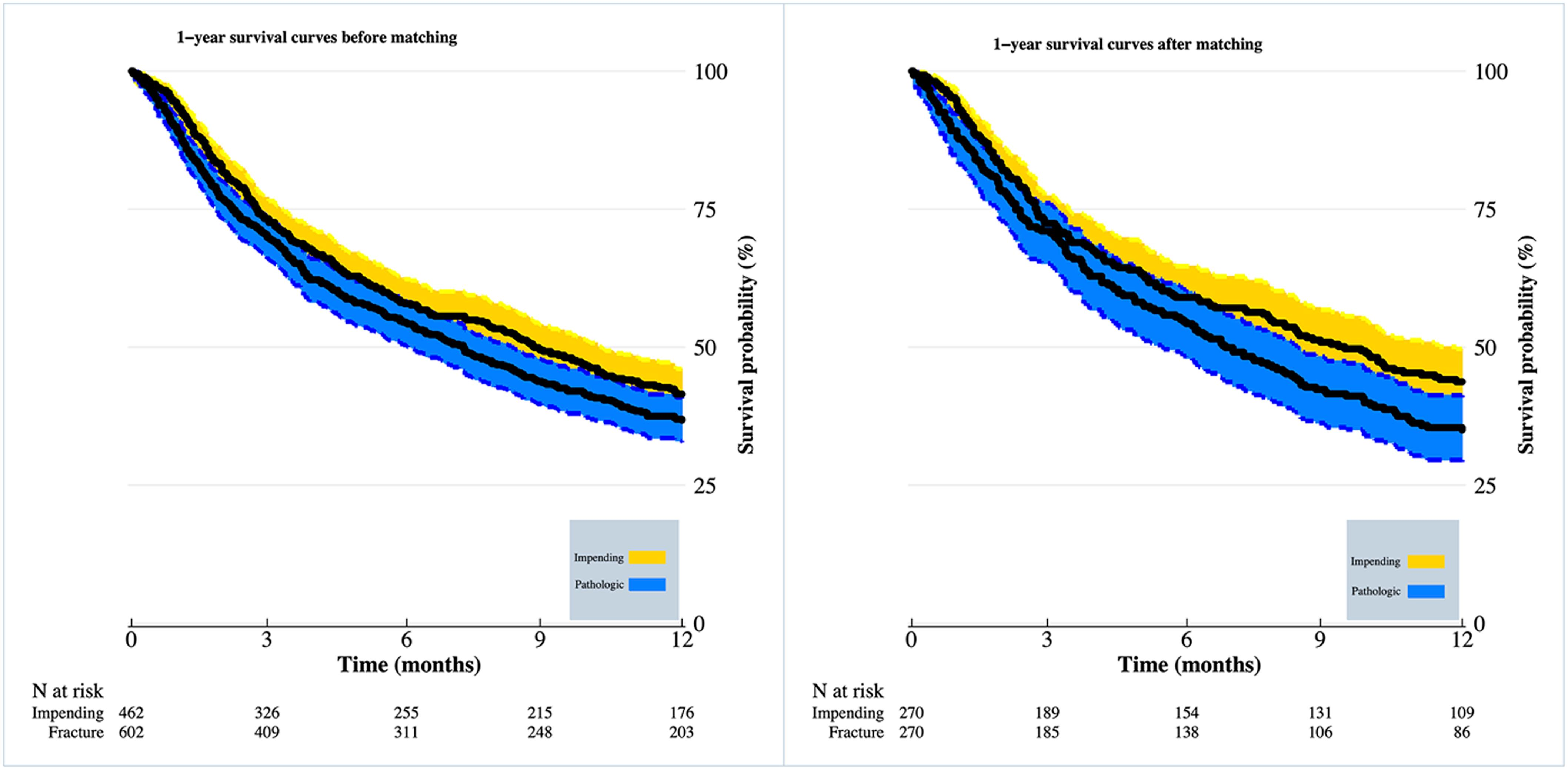
The international multicenter study by Schutgens et al. in the October 7, 2020 issue of JBJS reports findings from an analysis of >300 cases of
A technique that combines magnetic resonance (MR) imaging with high-intensity focused ultrasound hyperthermia provides faster pain relief than conventional radiation therapy (RT) for patients with
Every month, JBJS publishes a Specialty Update—a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 13 subspecialties.