Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, author
Tag: tumor resection
The international multicenter study by Schutgens et al. in the October 7, 2020 issue of JBJS reports findings from an analysis of >300 cases of
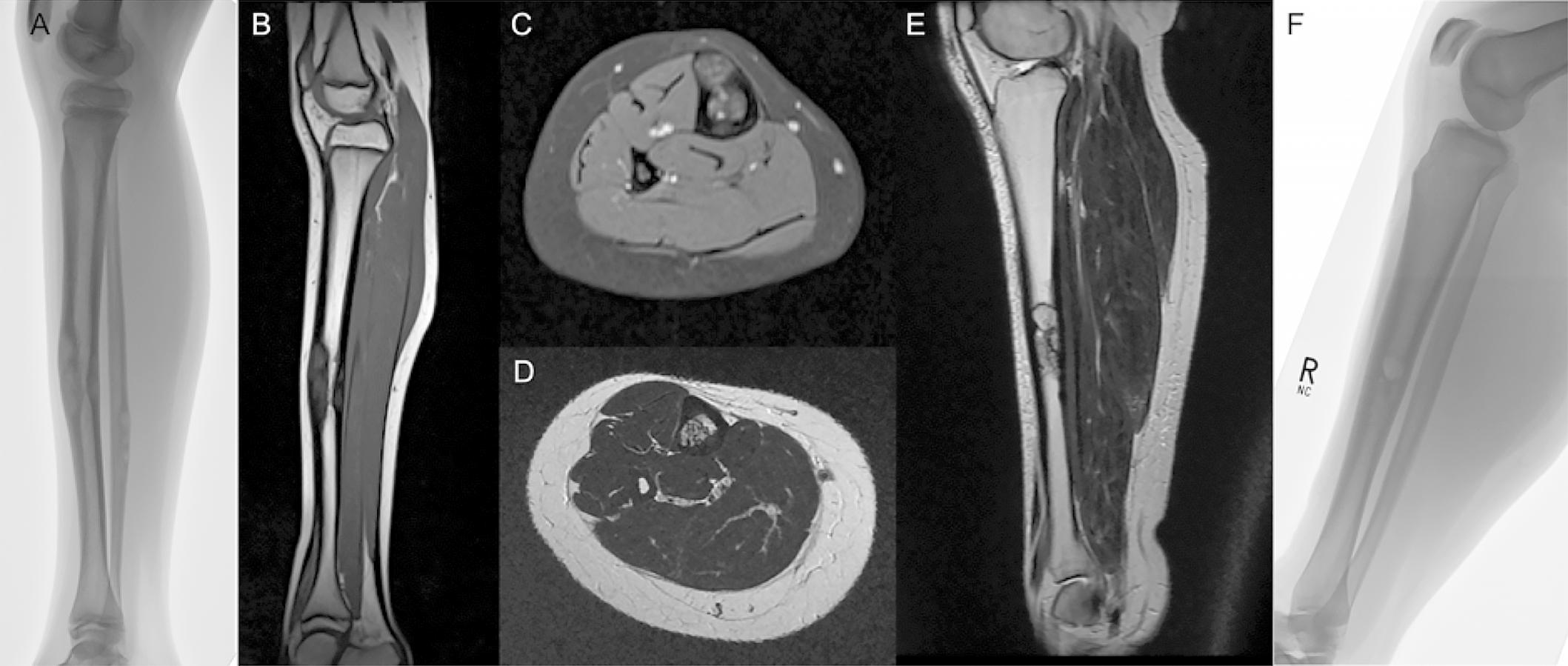
Resection of long-bone tumors often leaves large skeletal defects. Since the late 1980s, surgeons have used the “hybrid” Capanna technique—a vascularized fibular graft inlaid in