The use of computer navigation in total joint arthroplasty is increasing. Navigation has been employed less in total hip arthroplasty (THA) than in total knee arthroplasty, perhaps because of the increased need for image-based navigation in THA, leading to increased cost, time, and radiation. However, with options for imageless navigation becoming available for THA, it is reasonable to deduce that usage will increase. Research has shown that the use of navigation improves acetabular cup positioning, but there is a paucity of literature looking at the effect of computer navigation on implant survival.
In the current issue of JBJS, Agarwal et al. present the results of their analysis of data from the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR), in which they examined the impact of computer navigation on the rates of all-cause revision and revision for dislocation following THA. They included only modern bearing surfaces and excluded metal-on-metal surfaces (because of their known high rate of revision) as well as dual-mobility and constrained liners.
Their findings? During the study period (2009 to 2019), registry data showed 269,848 THAs performed for osteoarthritis. Of these, 6,912 (2.6%) utilized computer navigation. The use of navigation increased from 1.9% of all primary THAs in 2009 to 4.4% in 2019.
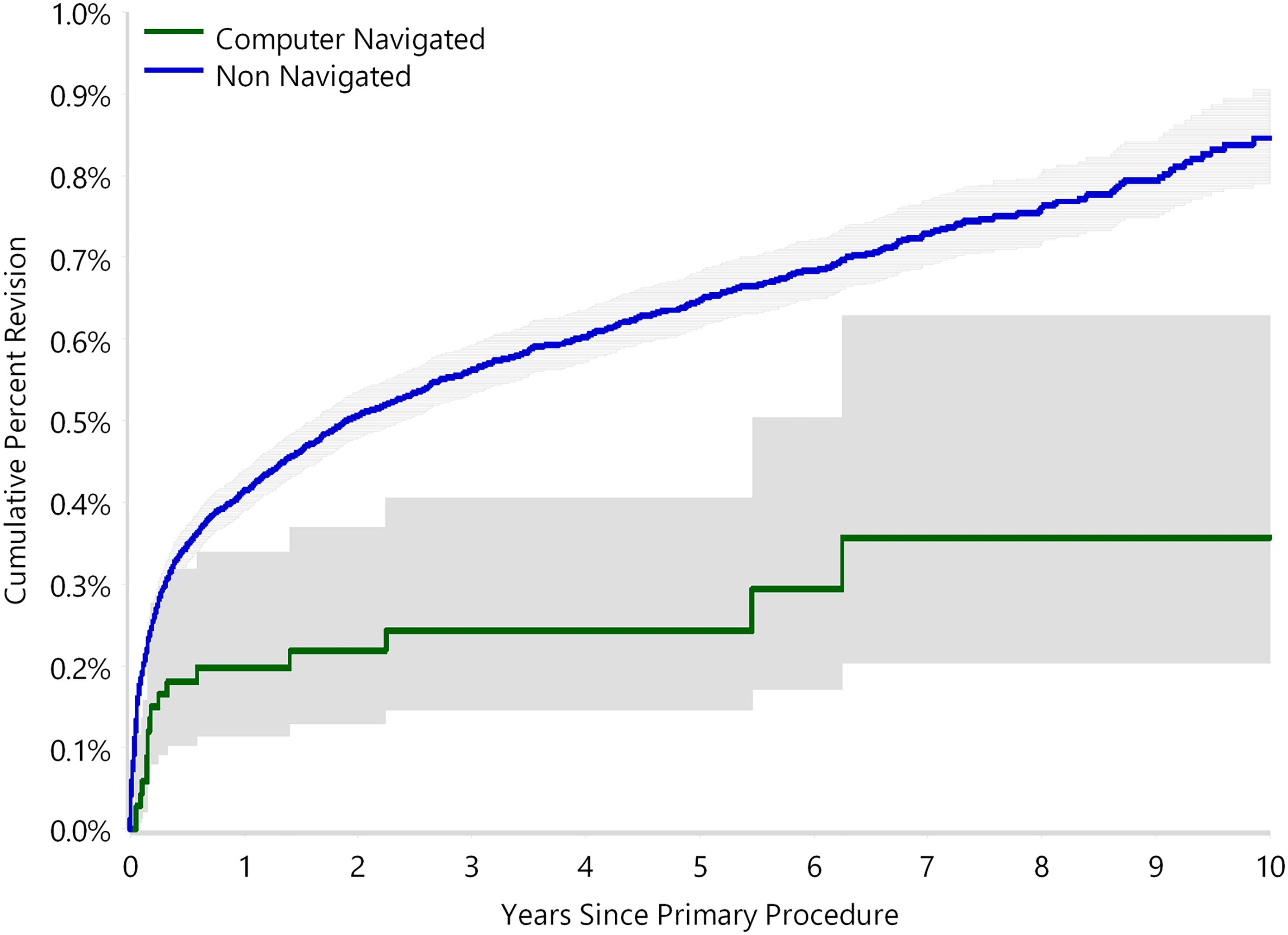
No significant difference in the rate of all-cause revision was found when comparing navigated and non-navigated cases (cumulative percent revision at 10 years of 4.0% and 4.6%, respectively).
However, navigation demonstrated a significantly lower rate of revision for dislocation (0.4% versus 0.8%; HR, 0.46; p = 0.002). There was no difference in the revision rate based on surgical approach (data collected since 2015 showing 4,209 THAs performed with navigation and 140,582 without navigation).
A subanalysis of the 5 most commonly used component combinations yielded a significantly lower rate of all-cause revision for navigation (2.4% vs 4.2%; HR, 0.64; p = 0.003). The authors also found that, among surgeons who performed both navigated and non-navigated THAs, there was a lower rate of revision for dislocation for navigated THAs (0.4% vs. 0.8%; HR, 0.49; p = 0.004).
Registries like the AOANJRR—which accounts for nearly 100% of all joint arthroplasties performed in Australia—are important for looking at “big data.” And with these large data sets, researchers can analyze outcomes of orthopaedic procedures for a multitude of purposes. As the authors rightly note, however, “although this study has the strength of a national registry representing a national population, we cannot infer causation.” Large, randomized clinical trials can help us better answer research questions that large data sets reveal, and ultimately improve the care of our patients.
Read the full report here.
Matthew R. Schmitz, MD
JBJS Deputy Editor for Social Media