Applications are now being accepted for the Hip Diploma Online Course from JBJS and MRC Oxford. The online course starts Monday, May 19, and will
Category: Education and Training
JBJS Clinical Classroom continues to grow as a learning hub. Clinical Classroom subscribers now have access to JBJS Chapman’s Comprehensive Orthopaedic Surgery, an indispensable resource

These 42 US-based journal clubs were recently awarded funding by JBJS to enhance their journal club activities. Journal clubs use the JBJS award funds in
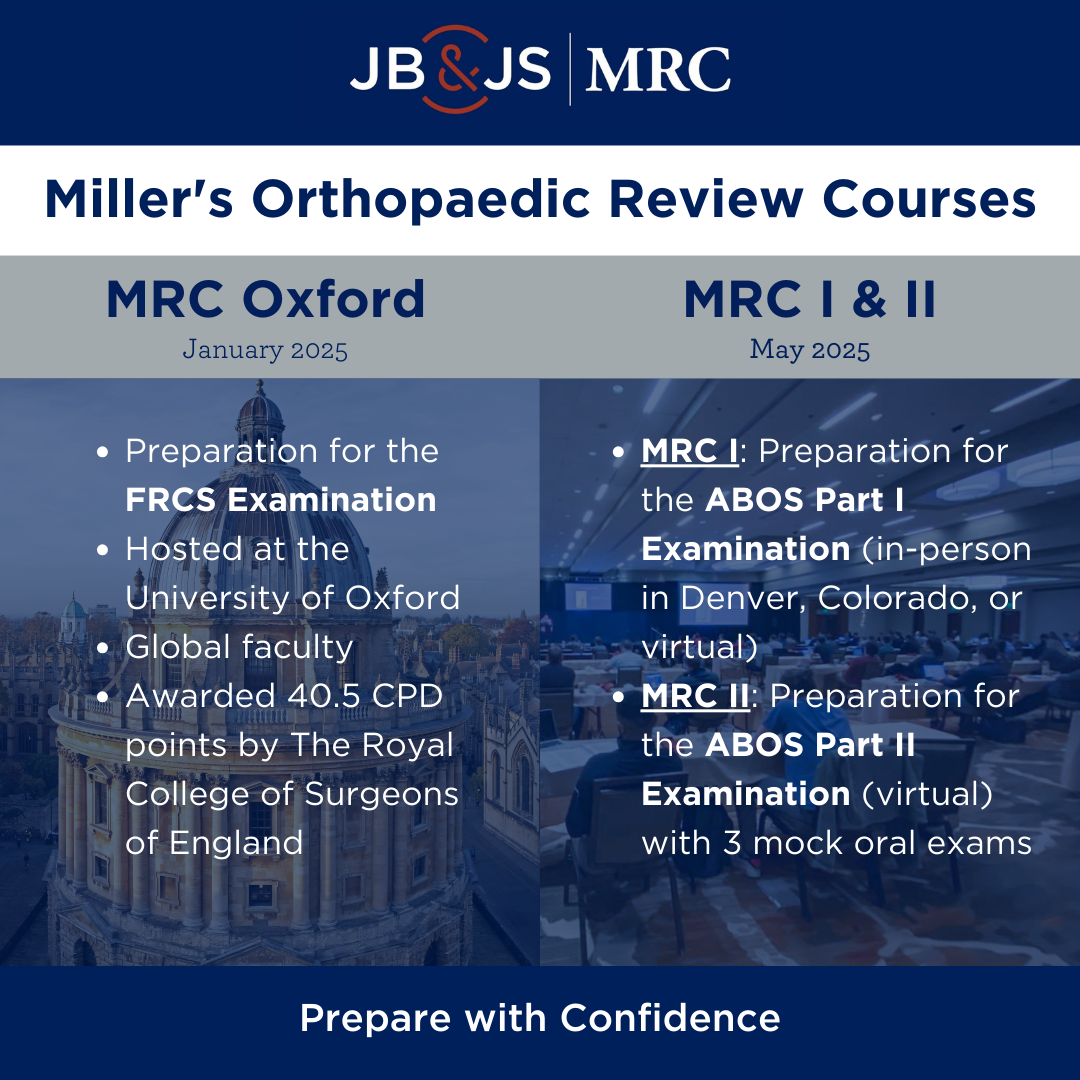
Whether you’re preparing for the ABOS or FRCS exam, JBJS has two outstanding educational programs available to residents and early-career surgeons. Prep Courses for the

This Resident Roundup post comes from Matt Hess, MD, who is a fellow in orthopaedic oncology at The University of Chicago. Moving across the country

This guest post is from Artina Dawkins, PhD, MPA, C-TAGME, and Holly Pilson, MD. Dr. Dawkins is the Co-Director of Diversity and Inclusion & Program

A total of 48 US-based journal clubs received JBJS funding support in October 2023 to enhance journal club resources and activities. Among the recipients were

This Resident Roundup post comes from John Ibrahim, MD, who is a PGY5 orthopaedic resident at Albert Einstein Healthcare Network, in Philadelphia, Pennsylvania. He will

This Resident Roundup post comes from Mike Kim, MD, an incoming intern in the Department of Orthopaedic Surgery at the University of California, Irvine School

In a recent article in JBJS, Escalera et al. provide an informative overview of the American Association of Latino Orthopaedic Surgeons (AALOS). Since its founding