Early hip arthroscopists routinely performed capsulectomies to obtain adequate visualization within the hip joint. As our techniques and skills have evolved, more modern capsulotomies are now employed, and with that transition in techniques has come a debate over whether or not to repair, or close, the capsule. Some cadaveric studies have demonstrated that an unrepaired capsule can lead to increased instability in multiple planes and increased axial distraction. However, in terms of clinical utility, while some studies have demonstrated an improvement in mid-term patient-reported outcomes after capsular repair, others have found no difference in outcomes between patients with and without repair. At the same time, there are limited in vivo data on the effect of different capsular repair techniques.
Shedding new light on the topic is a report by O’Neill et al. in the current issue of JBJS. The investigators studied how capsular repair affects axial distraction during hip arthroscopy using an in vivo intraoperative testing model. Included were 31 patients (23 female and 8 male) who were undergoing primary hip arthroscopy for femoroacetabular impingement (FAI) performed by a single surgeon. The mean age of the patients was 32.7 years.
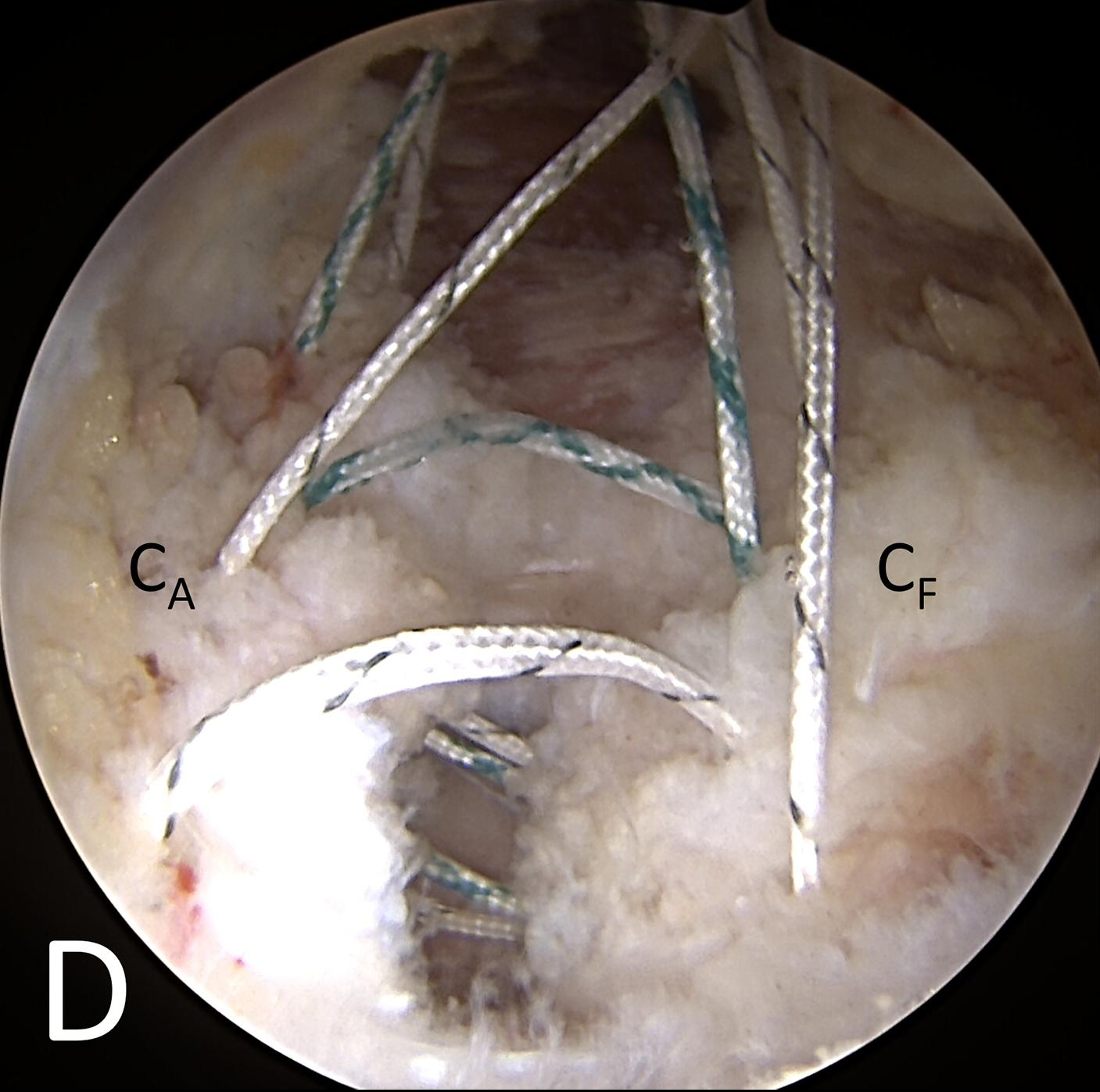
The authors measured the distance between the femoral head and the lateral edge of the sourcil at increasing amounts of traction, 12.5-lb (5.7-kg) increments, up to 100 lbs (45.4 kg). Fluroscopic images were made at each traction interval in 3 hip states: (1) prior to instrumentation; (2) after the performance of the interportal capsulotomy, labral repair, and osteochondroplasty; and (3) following repair of the capsule. Capsular repair was performed using a figure-of-8 suture configuration (29 of 31 patients received 3 sutures, and 1 patient each received 2 and 4 sutures). There were no T-type capsulotomies.
Capsulotomy resulted in significant increases in distraction distance from 25 to 100 lbs of traction compared with both baseline (native hip) and repair states. The capsular repair state was similar to the native capsule at all traction increments, with the exception of 37.5 and 50 lbs., where the distraction distance was significantly greater for capsular repair, but this difference did not persist when traction time was controlled for.
The authors concluded that “This in vivo model demonstrates that an unrepaired interportal capsulotomy significantly increases axial distraction distance compared with the native, intact hip capsule.”
As our techniques in hip arthroscopy continue to improve, so do our management skills regarding the joint capsule. If the goal of FAI surgery is to restore or create normal anatomy by fixing the acetabular labrum and reshaping the proximal femoral head-neck junction, we will need to continue to study the effects of restoring the natural capsular anatomy as well. Future studies can focus on clinical outcomes in this realm to see whether restoring all anatomy in the treatment of FAI leads to improvements in function.
Additional perspective on this study is provided in the related Author Insights video. Access the video here.
An up-close look at capsular closure and related discussion on the procedure are presented in a recent JBJS Essential Surgical Techniques article by Economopoulos et al. Click here to access this video-based article.
Matthew R. Schmitz, MD
JBJS Deputy Editor for Social Media



We are going back to restore the normal anatomy as far as possible for the near normal hip functions