The majority of patients who undergo primary total hip arthroplasty (THA) and total knee arthroplasty (TKA) are discharged to home postoperatively, but for some patients, discharge to a higher level of care such as a skilled nursing or inpatient rehabilitation facility may be more appropriate. Such decisions are complex. Discharge to a non-home setting is associated with not only higher costs but increased complication and readmission rates. Being able to predict the most appropriate discharge disposition prior to surgery or in the immediate postoperative period can help facilitate more efficient patient-care transitions while lowering costs and risks of complications.
As reported in the February 16, 2022 issue of JBJS, Hadad et al. evaluated the predictive ability of 2 tools to determine the discharge disposition of patients undergoing primary THA and TKA: the Predicting Location after Arthroplasty Nomogram (PLAN) and the Activity Measure for Post-Acute Care (AM-PAC) “6-Clicks” score.
PLAN, which is administered preoperatively, predicts the chances of not returning to home using several variables including demographic factors, factors related to the home setting, and clinical history. It has been externally validated but has not been previously evaluated in a large-scale study. The AM-PAC “6-Clicks” score, administered postoperatively, assesses the level of assistance a patient requires for 6 basic mobility skills. It has been used to predict discharge disposition after both orthopaedic and nonorthopaedic procedures.
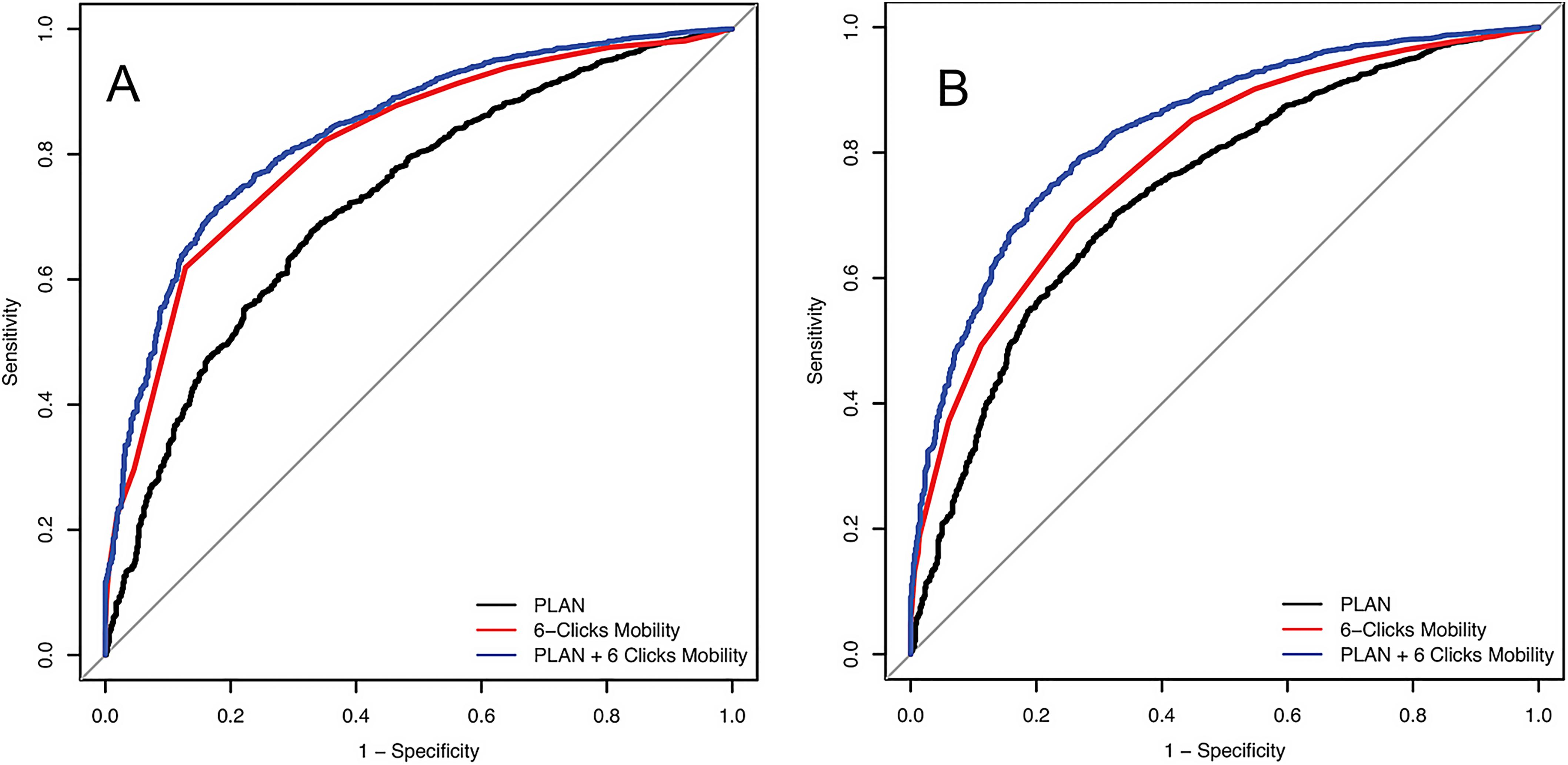
The study by Hadad et al. included 11,672 patients (4,923 THA and 6,749 TKA) from a single large hospital system. Both PLAN and “6-Clicks” scores were recorded for all patients. The authors constructed regression models and receiver operator characteristic curves to evaluate the prediction concordance of the tools with the actual discharge disposition (home or a facility).
Interestingly they found a reduction in the rate of non-home discharge over the course of the study, especially in the last year of the study (data was collected from December 2016 through March 2020). This could be related to an increase in focus on cost containment, but perhaps also an increased focus on optimization. The authors note the COVID-19 pandemic as one potential contributor this finding.
In terms of statistical findings, PLAN scores showed good discrimination in predicting home discharge, as demonstrated by a concordance index of 0.723 for the THA cohort and 0.738 for the TKA cohort. The “6-Clicks” scores assessed within the first 48 hours postoperatively showed excellent discrimination for the THA cohort (0.813) and good discrimination for the TKA cohort (0.790). And when the tools were used together, excellent concordance statistics were found (0.836 for both THA and TKA).
The authors also observed that when the tools agreed on home discharge, there were higher rates of discharge to home (98.0% for THA and 97.7% for TKA) and lower readmission rates (5.1% for THA and 7.0% for TKA) than when the tools disagreed. When the tools disagreed on discharge disposition, the authors observed a higher rate of readmission and a lower rate of discharge to home, leading them to conclude that “both preoperative and postoperative variables are important to consider in the determination of discharge disposition.”
Further work to externally validate this study is needed, but I commend the authors on combining both preoperative and postoperative analytic tools in this large-volume study. Such data can perhaps help us in refining the ability to predict discharge disposition to best address the postoperative needs of our arthroplasty patients.
Matthew R. Schmitz, MD
JBJS Deputy Editor for Social Media
A related commentary article by Amit Meena, MBBS, MS, DNB provides additional perspective on this study.