The opioid crisis in America has been well documented. The CDC reports that estimated deaths from drug overdoses topped 100,000 in 2021. Estimated deaths involving opioids increased to >80,000 (up from approximately 70,000 in 2020)1.
As noted in a new JBJS report by Krakow et al., opioids represent the fastest-growing drug problem among U.S. children and adolescents. In addition, exposure to opioids in adolescence may predispose individuals to addiction as adults.
How have prescribing patterns changed in response to the epidemic? The investigators shed helpful light on the topic.
Trends in Opioid Prescribing for Nonoperative Pediatric Injuries
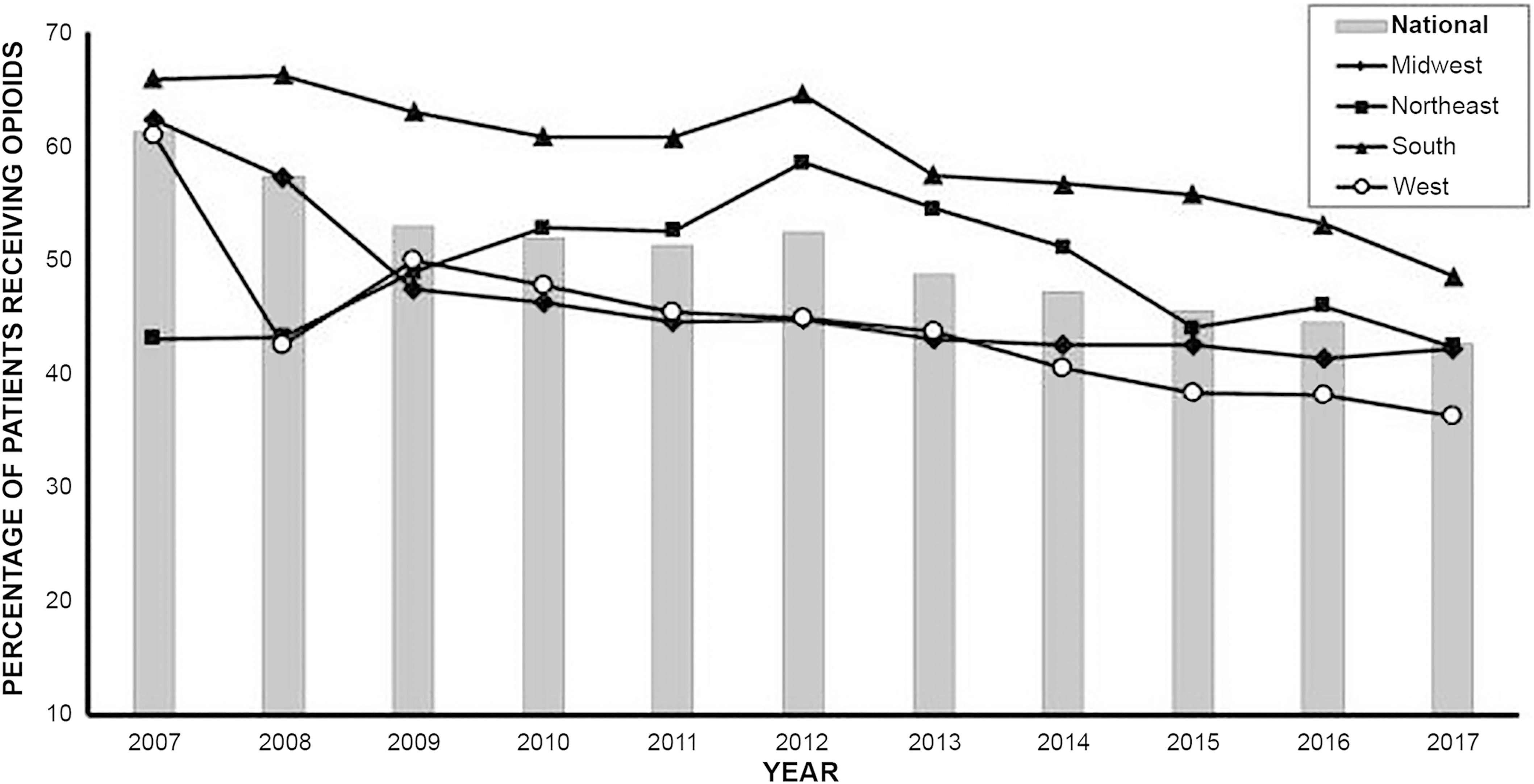
Krakow et al. studied trends in opioid prescribing from 2004 to 2017. Regional trends were evaluated from 2007 to 2017.
The authors retrospectively reviewed the Pediatric Health Information System (PHIS) database. Data from 42 participating hospitals were analyzed. Included were pediatric patients with the 10 most common fractures and dislocations treated on an outpatient basis with nonsurgical management.
- The final cohort included 134,931 patients with an average age of 12.6 years (range, 10 to 18 years). Nearly 70% of the patients were male.
- Overall, 69,740 (51.7%) of the patients were prescribed at least one dose of opioid in their ED or clinic visit.
- The national opioid prescription rate dropped significantly from 2007 to 2017, from 61.3% to 42.6% (p < 0.001).
- Regional differences were observed. Patients in the South were 71% more likely and patients in the Midwest were 26% more likely to receive an opioid prescription compared to patients in the Northeast. These differences were significant in unadjusted estimates, but nonsignificant after adjusting for variation among hospitals.
- In terms of demographics, adolescent patients ages 13 to 17 were 16% (95% CI, 13.10% to 18.87%) more likely to receive an opioid prescription compared to patients ages 10 to 12. The authors noted racial differences as well, with Black patients being 17% (95% CI, 13.33% to 20.3%) less likely to receive an opioid prescription compared with White patients. The authors state that there are a number of factors that likely contribute to this finding, including provider bias and underlying racial stereotypes.
Achieving Further Momentum
With increased recognition of the opioid epidemic, we’re seeing movement in the right direction with the overall decrease in prescribing. Nonetheless, we as an orthopaedic community can do better. There are regional differences and more alarmingly, racial differences that warrant further study and represent health-care disparities that we need to address.
I would also argue that the 2017 rate of >40% of children and adolescents receiving opioid medication for nonoperatively managed fractures and dislocations is still far too high. As surgeons, we need to work together with our patients, and with families, on education regarding the dangers of narcotic pain medications, while also employing non-narcotic options to relieve pain and discomfort.
Access the full JBJS report by Krakow et al.
Matthew R. Schmitz, MD
JBJS Deputy Editor for Social Media
References
- Centers for Disease Control and Prevention. National Center for Health Statistics. U.S. Overdose Deaths In 2021 Increased Half as Much as in 2020 – But Are Still Up 15%. 2022 May 11. https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm