A number of measures have been suggested for reducing perioperative blood loss (PBL) in total hip arthroplasty (THA). A new randomized clinical trial in JBJS assesses the efficacy of bone wax application in reducing PBL in total hip arthroplasty performed via the direct anterior approach.
Study Highlights
- This triple-blinded, Level-I study by Mortazavi et al. was performed at the Joint Reconstruction Research Center, Tehran University of Medical Sciences, Tehran, Iran.
- Included were 152 patients who underwent THA via the direct anterior approach. In 75 patients, bone wax was applied on the surface of the distal part of the femoral neck following osteotomy, and in 77 patients (control group), no bone wax was used.
- The mean age of the patients was 47.7 years; 50.7% of the patients were female, and 49.3% of the patients were male. Demographics and baseline hematologic variables did not differ between the groups.
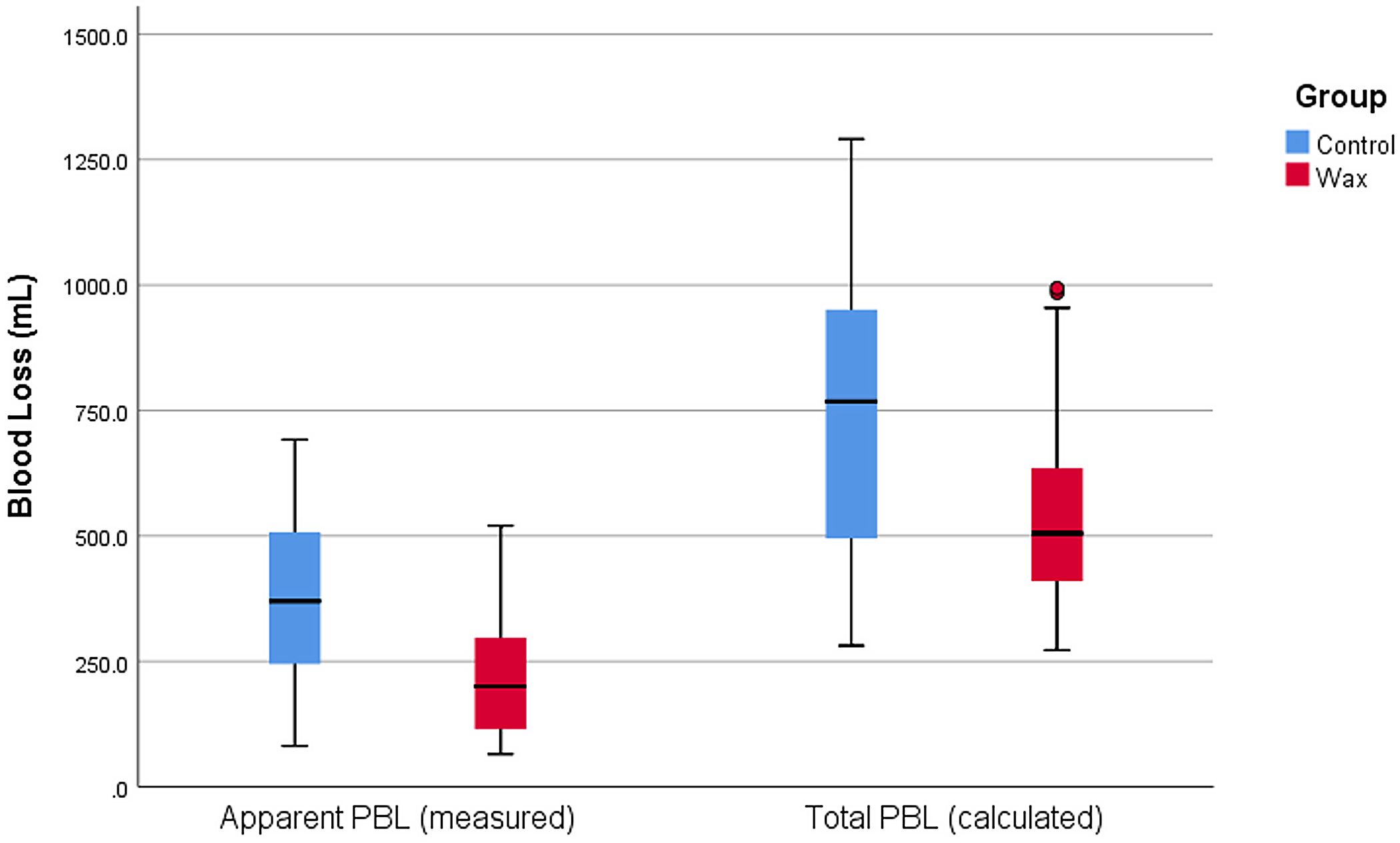
- The primary outcomes were apparent PBL (blood in sponges and the suction canister) and total PBL on postoperative days 3 and 5. Secondary outcomes were transfusion and complications.
Findings
The authors found that apparent PBL, total PBL on postoperative day 3, and total PBL on postoperative day 5 were significantly lower in the group treated with bone wax. The corresponding median values (in millimeters) were as follows: 200 (IQR, 115 to 310) vs. 370 (IQR, 195 to 513.7); 505.2 (IQR, 409.2 to 637.6) vs. 747 (IQR, 494.6 to 955.4); and 536.7 (IQR, 430.9 to 689.3) vs. 767.8 (IQR, 537.8 to 1,021.9) in the wax and control groups, respectively (p < 0.001 for all).
The authors found no significant difference between the 2 groups in the rates of transfusion and complications.
They note that their described technique is not intended for surgeons who broach the femur first. They conclude that “bone wax on the distal cut surface of the femoral neck during THA through the direct anterior approach can significantly reduce PBL. It is practical, readily available, and inexpensive and could be considered as a routine part of the surgical technique in THA through the direct anterior approach.”
Access the full JBJS report: The Efficacy of Bone Wax in Reduction of Perioperative Blood Loss in Total Hip Arthroplasty via Direct Anterior Approach. A Prospective Randomized Clinical Trial



I will not draw too much attention to the choice of a radiograph of a pelvis with bipolar hemiarthroplasty in an article involving total hip arthroplasties (THAs).
I will comment about my surprise, not about how well the bone wax worked at haemostasis of a bleeding bone but how much blood loss can occur from a femoral neck cut. Keeping in mind the excellent operative time of less than 80 minutes, with a well oiled scrub team, I was not expecting that the potentially preventable blood loss from the femoral neck can be more than 1 unit of blood as suggested by this study. It certainly made me reassess my practice.
The advent of new surgical and anaesthetic techniques, combined with medications like TXA certainly made a great difference in blood loss from THA over the last 2 decades; blood transfusion for patients post primary THA is now the exceptions rather than the norm.
While bone wax has been in use over 100 years to stop bleeding (1), and while bone wax has been described in elective THAs for purpose of both volumetric determination of bone defects (2) as well as haemostasis from femoral neck osteotomy (3), hence not a novel idea, but this is the first time as far as I am aware, that the amount of blood loss (that can be addressed by bone wax application) is actually quantified.
The authors should be congratulated for their contribution to evidence-based medicine; the key now is no longer about what is the evidence, but whether enough surgeons take up the practice. Bone wax application does have its own complications and concerns, particular exotic infections (1,4); there are possibilities of bone wax substitutes although there are none currently available nor commercially viable as far as I am aware. Perhaps this may be the only final barrier to its wide-spread use.
References
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6551357/
2. https://pubmed.ncbi.nlm.nih.gov/34898037/
3. https://pubmed.ncbi.nlm.nih.gov/24780681/
4. https://pubmed.ncbi.nlm.nih.gov/33593449/
Thank you for your comment. The image that previously accompanied this post has been updated. A figure from the study discussed is now shown.