In this OrthoBuzz post, Editor-in-Chief Dr. Marc Swiontkowski reflects on a new JBJS study that examines pain catastrophizing among patients with adolescent idiopathic scoliosis (AIS).
Over the last 5 to 7 years, we have seen an increase in JBJS submissions that expand our working knowledge of how patient factors impact functional outcomes of invasive orthopaedic procedures. Among these factors being explored are psychological factors such as depression as well as pain catastrophizing (a cognitive tendency to have negative thoughts and feelings about pain).
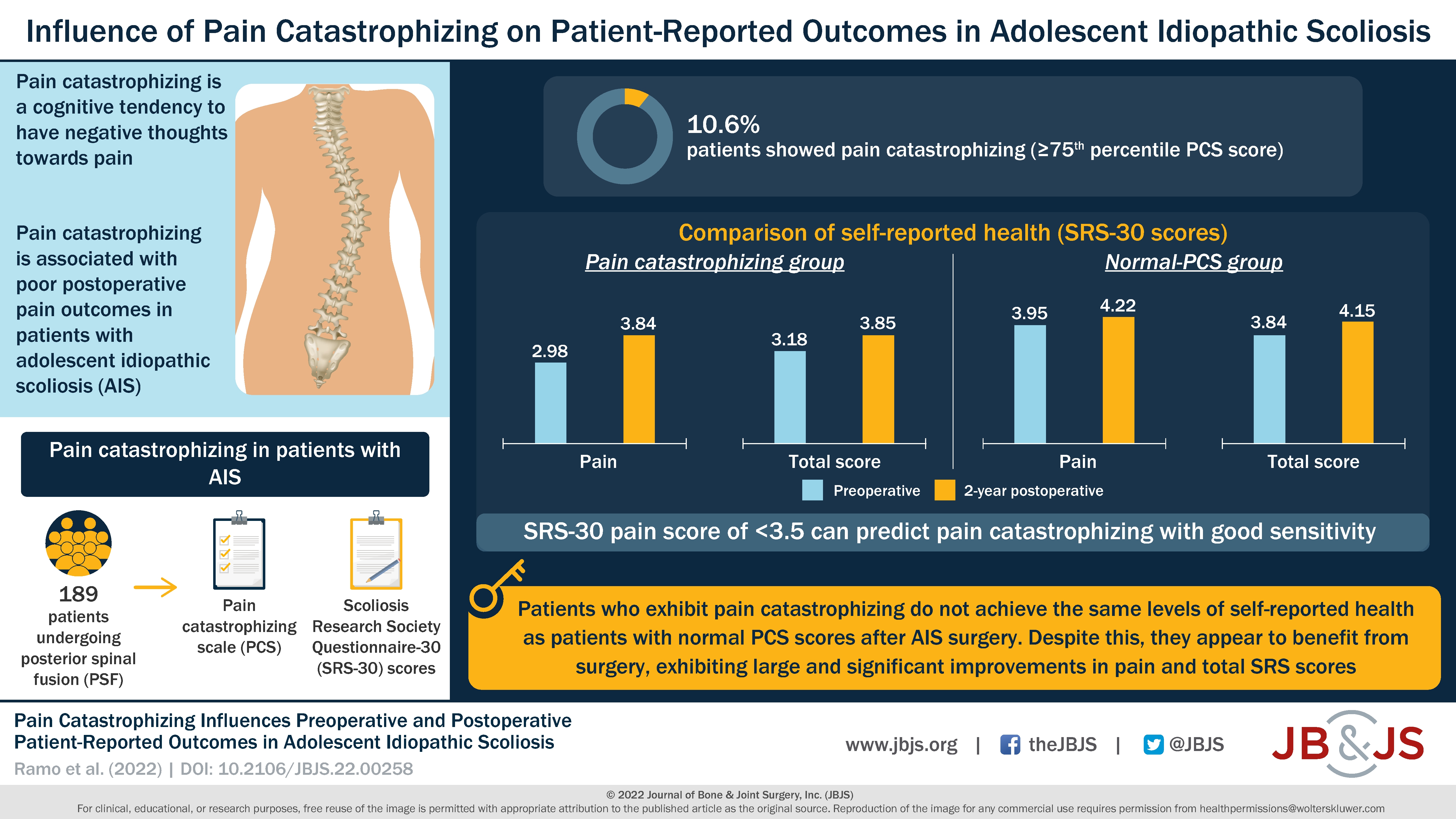
The majority of this research has involved adult patients. However, in the current issue of JBJS, Ramo et al. report on the impact of pain catastrophizing on patient-reported outcomes in a cohort of 189 adolescent patients undergoing posterior spinal fusion for AIS.
Study Highlights
- Twenty of the 189 patients (10.6%) experienced clinically relevant pain catastrophizing. This was defined as Pain Catastrophizing Scale for Children (PCS) score in the 75th percentile or higher (PCS ≥30).
- The preoperative PCS score was evaluated in relation to preoperative and 2-year postoperative scores of the Scoliosis Research Society Questionnaire-30 (SRS-30), which assesses health-related quality life.
- Patients who demonstrated pain catastrophizing experienced significant improvement in their self-reported health at 2 years after surgery (including a clinically relevant improvement in pain). However, when compared with patients with a normal PCS score, those in the pain-catastrophizing group had significantly lower preoperative SRS-30 scores (pain, appearance, activity, mental health, and total score).
- At 2 years postoperatively, the pain-catastrophizing group continued to have lower SRS-30 scores, including significantly lower pain and total scores, compared with the normal-PCS group.
- A receiver operating characteristic (ROC) curve analysis found that an SRS-30 pain score of <3.5 showed good sensitivity for predicting pain catastrophizing.
The authors concluded that “clinically relevant pain and pain catastrophizing before surgery for AIS may predict greater self-reported pain and lower scores on other self-reported outcomes 2 years postoperatively.” They suggest that systems to identify pain catastrophizing preoperatively “may assist surgeons in making appropriate referrals for preoperative psychological counseling and ultimately enable patients to have better postoperative outcomes.”
This investigation should encourage clinical researchers across musculoskeletal conditions and interventions to build on data-collection efforts to assess pain perception as an important variable and its impact on functional outcomes.
Access the full report by Ramo et al., including a downloadable infographic.
Marc Swiontkowski, MD
JBJS Editor-in-Chief