In this post, JBJS Editor-in-Chief Dr. Marc Swiontkowski reflects on the growth of Medicare Advantage enrollment and the impact it may have on orthopaedic database research.
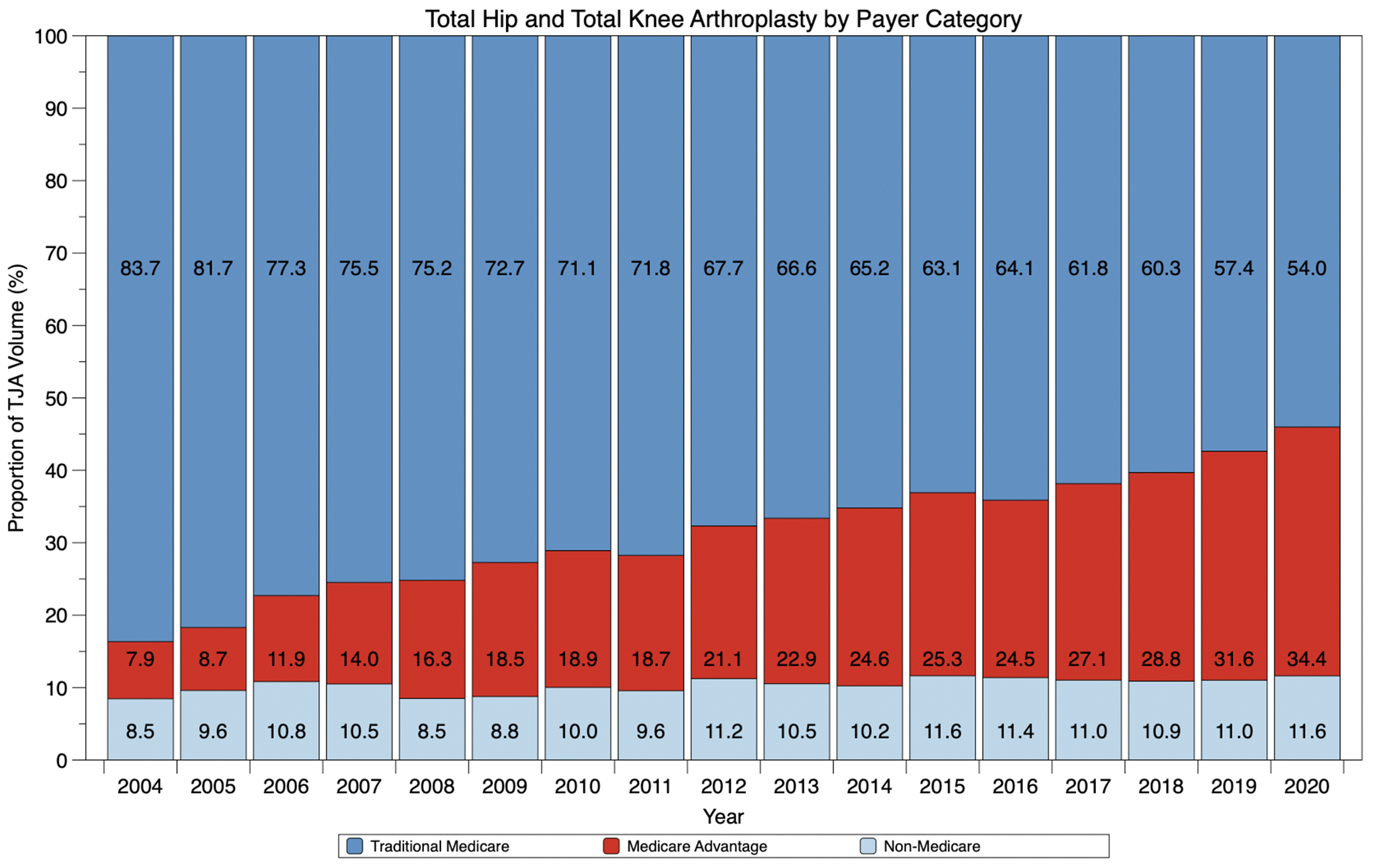
Medicare-eligible patients have increasingly moved to privatized Medicare Advantage plans. In a new JBJS report, Wang et al. examine the rise of Medicare Advantage among patients ≥65 undergoing primary elective total joint arthroplasty (TJA). Using the Premier Healthcare Database, they found that the proportion of patients with Medicare Advantage increased from 7.9% in 2004 to 34.4% in 2020. In that same period, the proportion with traditional Medicare decreased from 83.7% to 54.0%.
While patients seem to be finding benefit in moving from traditional CMS management of benefits to large private insurers (potential cost savings, perceived ease of care-decision management), there are additional considerations worthy of our attention. The Advantage program comes with the pre-approval structure that is in place for commercial insurance plans, which can result in delays in operative care decisions. Furthermore, as Wang and colleagues point out, the requirement for prior authorization places an increased administrative burden on orthopaedic practices.
Impact on Database Research
It’s also important to consider how the move toward Medicare Advantage could impact access to data for studies of long-term orthopaedic outcomes (reoperations, revision, survivorship, etc.). With the shift in benefits management to private insurers, comprehensive data residing in the CMS data set may thus be reduced. This has already resulted in less fidelity of the data set for large database research. JBJS recently published the supplement “Large Database and Registry Research in Joint Arthroplasty and Orthopaedics,” which explores the power and potential of large databases in orthopaedic investigations. This important caveat regarding the use of the CMS data is contained therein.
Wang et al. also discuss this associated research impact in their report. And they note that organizations reliant on traditional Medicare data to inform health-care policy decisions could be similarly affected.
Looking more closely at their study findings:
- Of the 697,317 included patients who underwent primary elective TJA from 2015 to 2020, 67.6% had traditional Medicare coverage and 32.4% were covered by Medicare Advantage. While the groups were similar in age and sex, a higher proportion of Black patients (8.29% compared with 4.62%; p < 0.001) and a lower proportion of White patients (84.0% compared with 89.2%; p < 0.001) were enrolled in Medicare Advantage compared with traditional Medicare.
- An analysis of postoperative complications found that enrollment in Medicare Advantage was associated with higher odds of surgical site infection, periprosthetic joint infection, stroke, and acute kidney injury, but lower odds of urinary tract infection.
They investigators state that it is essential to understand the causes of the increased complication rates, “as greater complications along with the greater administration burden associated with MA [Medicare Advantage] plans may deepen social disparities in arthroplasty care and limit registry-based outcome assessment.”
I agree with the authors that further study of insurance utilization trends is needed so that we can better understand the impact on patient populations, outcomes, and costs. In addition, orthopaedic researchers need to be aware of changing insurance utilization patterns in terms of the related challenges to database research.
Additional perspective on this study is provided in the related Author Insights video and in a commentary by James A. Keeney, MD.
JBJS Editor-in-Chief