Hip preservation surgery has become increasingly popular over the last decade, and we continue to learn more about appropriate indications and patient selection. For hip dysplasia, a periacetabular osteotomy has been shown to alter the natural history and delay the onset of arthritis. Treatment of those with impingement symptoms and borderline hip dysplasia (BHD), however, may be more difficult. Recent advances in arthroscopic management of the capsule have shown good short- to intermediate-term results in patients with BHD. Nonetheless, there is concern that subtle instability could become worse with hip arthroscopy alone.
In the current issue of JBJS, Domb et. al. report minimum 10-year survivorship and patient-reported outcome measures (PROMs) following primary hip arthroscopy with capsular plication and labral preservation in patients with BHD and a labral tear and/or femoroacetabular impingement syndrome.
Of 56 hips eligible for evaluation, 45 hips (80.4%) had minimum 10-year follow-up (range, 120.0 to 142.3 months; 38 hips in female patients and 7 in male patients). BHD was defined as a lateral center-edge angle between 18° and 25°. Baseline and minimum 10-year PROM scores were collected, with measures including the modified Harris hip score (mHHS), Nonarthritis Hip Score (NAHS), Hip Outcome Score-Sports Specific Subscale (HOS-SSS), and visual analog scale (VAS) for pain. Exclusion criteria included any prior ipsilateral hip surgery, Tönnis osteoarthritis grade of >1, or a previous hip condition such as fracture, Legg-Calvé-Perthes disease, or osteonecrosis.
The investigators also compared the study group and a propensity-matched group of patients without BHD who had undergone primary hip arthroscopy. The groups were matched in a 1:2 ratio according to sex, age, body mass index (BMI), Tönnis grade, preoperative alpha angle, capsular treatment, and labral treatment.
Study Findings
In the study group of 45 hips, 8 patients underwent total hip arthroplasty (THA), for a 10-year survivorship rate of 82.2%. In the propensity-matched group of 90 hips, 7 patients underwent arthroplasty, for a survivorship rate of 92.2%. The difference in survivorship between the groups was not statistically significant.
The authors did find that, in the BHD group, patients with a BMI of ≥23 kg/m2 had 4.4 times (95% confidence interval [CI], 0.78 to 24.8 times) higher odds of undergoing conversion to THA and that patients ≥42 years of age had 7.1 times (95% CI, 1.4 to 37.2 times) higher odds of undergoing conversion to THA.
Both the BHD and matched control groups had significant improvements in PROM scores from preoperatively to 10 years. The 10-year scores did not differ significantly between the 2 groups. In addition, both groups met the criteria for the minimal clinically important difference (MCID) for each of the PROMs at similar rates:
mHHS – 79% (BHD); 79% (control)
NAHS – 79% (BHD); 77% (control)
HOS-SSS – 70% (BHD); 67% (control)
VAS for pain – 76% (BHD); 81% (control)
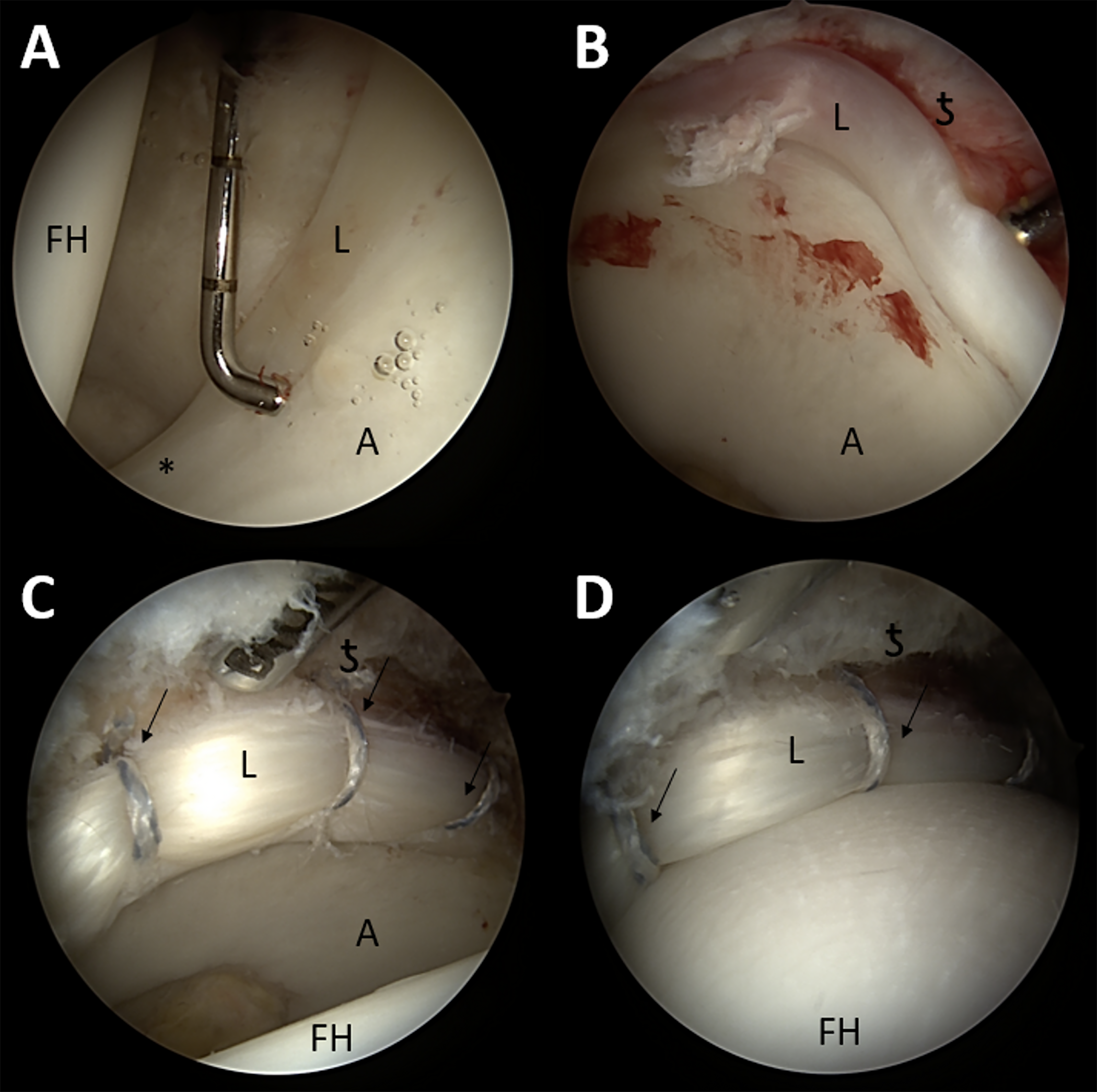
It is important to note that the senior author performed surgery with a capsular plication method that has been previously described.
Although this study is limited by small numbers and may have been underpowered to detect differences in survivorship, it does seem to show that, with meticulous surgical technique, lasting results can occur in patients undergoing hip arthroscopy in the setting of labral tears in BHD. Lacking in the current study are detailed preoperative clinical examination findings indicating instability or potential instability and how that may affect outcomes. In addition, it is unclear how other surgical procedures, such as femoroplasty, labral repair, and ligamentum teres debridement, might factor into outcomes. Although no patients required subsequent PAO for instability, it appears 3 patients included in the BHD cohort underwent PAO at the time of arthroscopy, and 3 hips (7%) required revision hip arthroscopy for recurrent labral tears in the BHD group.
Further studies are needed to tease out which patients with BHD would benefit from arthroscopy alone versus a combination of arthroscopy and PAO. But with advances in imaging and research collaboratives increasingly investigating the management of BHD, I am hopeful that some of the questions will be answered in the not-too-distant future.
Read the full study: Borderline Dysplasia After Primary Hip Arthroscopy with Capsular Plication and Labral Preservation: Ten-Year Survivorship and Patient-Reported Outcomes
JBJS Deputy Editor for Social Media




I think that about 38 years after the beginning of three-dimensional assessement of femoral head coverage, using wiberg’s angle to group border line dysplasia from others seems an odd approach of the problem.
Instability or coxo-femoral conflicts by impingment deserve three-dimensional assessement. So we can see that even tiny defects in coverage or malorientation of the acetabulum may be definitively managed by precise reorientation of the hip cup following a three-dimensional planning system.