JBJS is pleased to welcome Mary K. Mulcahey, MD as the new Deputy Editor for Sports Medicine, effective January 1 of this year. Dr. Mulcahey
Category: Uncategorized
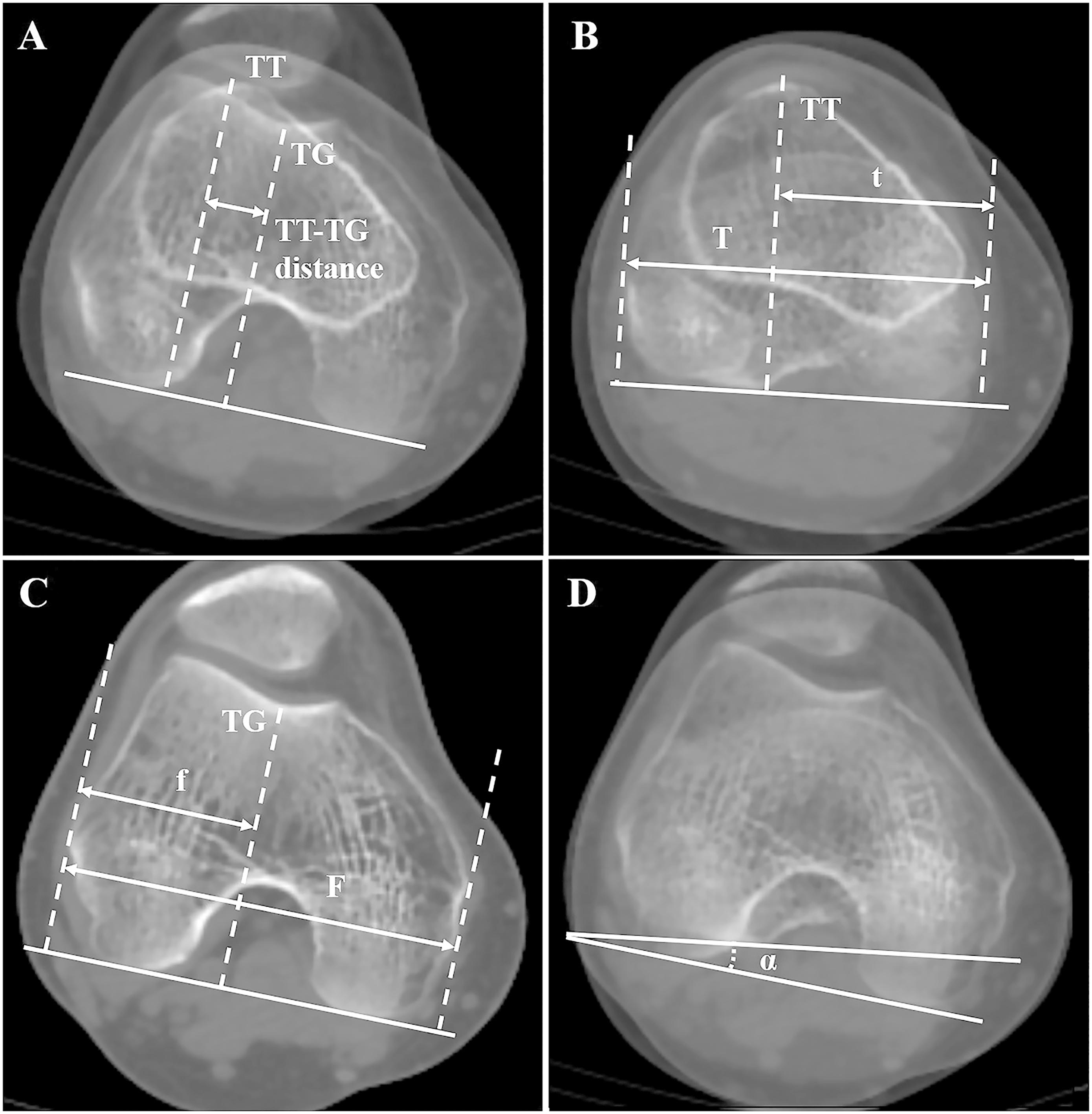
Patellar instability continues to be a focus of research, and there are numerous factors that potentially contribute to recurrent episodes of instability and functional loss.
Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, co-author

This commentary comes from guest contributor Matthew Deren, MD, in response to a recent study in The New England Journal of Medicine. To cement or
JBJS has expanded the popular “What’s Important” article series to include a new section focused on creativity entitled “What’s Important: Arts & Humanities.” In the

JBJS regularly publishes Current Concepts Review (CCR) articles, which provide concise and thorough reviews of the current literature on specific topics of interest to orthopaedic

This guest post comes from David Vizurraga, MD in response to a study in JAMA investigating platelet-rich plasma vs. placebo in the treatment of knee

Every month, JBJS publishes a review of the most pertinent and impactful studies from the orthopaedic literature during the previous year in 14 subspecialty areas. This month, co-author
Anterior cruciate ligament (ACL) injuries affect knee function and quality of life for thousands of young, active people every year. Surgeons reconstructing torn ACLs
JBJS will have a booth at the upcoming Annual Meeting in San Diego. The conference begins today, August 31, and runs until September 4. Stop

