Dr. Marc Swiontkowski, JBJS Editor-in-Chief, discusses a new study assessing the long-term outcomes of proximal humeral fractures sustained in adolescence.
Treating fractures involving the physes in children and adolescents has often been described in a positive light because of the generally great outcomes. There are, of course, the anxiety-producing fractures about the elbow (diagnostic concerns and risk of bad outcomes) and the knee and ankle (growth arrest leading to angular malunion and limb shortening). For the most part, however, fractures involving the physis in the proximal humerus are not as concerning. Nonetheless, we have lacked data on the long-term outcomes of these fractures and their management. Lähdeoja et al. address that issue in the current issue of JBJS:
Outcomes at a Mean of 13 Years After Proximal Humeral Fracture During Adolescence
In this study from Finland, the authors evaluated a large group of patients who had sustained a proximal humeral fracture when they were between the ages of 10 and 16 years. Included were patients treated surgically and non-surgically. Outcomes were assessed at a mean of 13 ± 3 years (range, 7.4 to 19.1 years).
The outcomes were simply outstanding, with essentially normal function found overall. This has to do with the advanced fracture-healing potential as well as the potential for remodeling in younger patients, as the proximal humerus growth plate has impressive biologic plasticity.
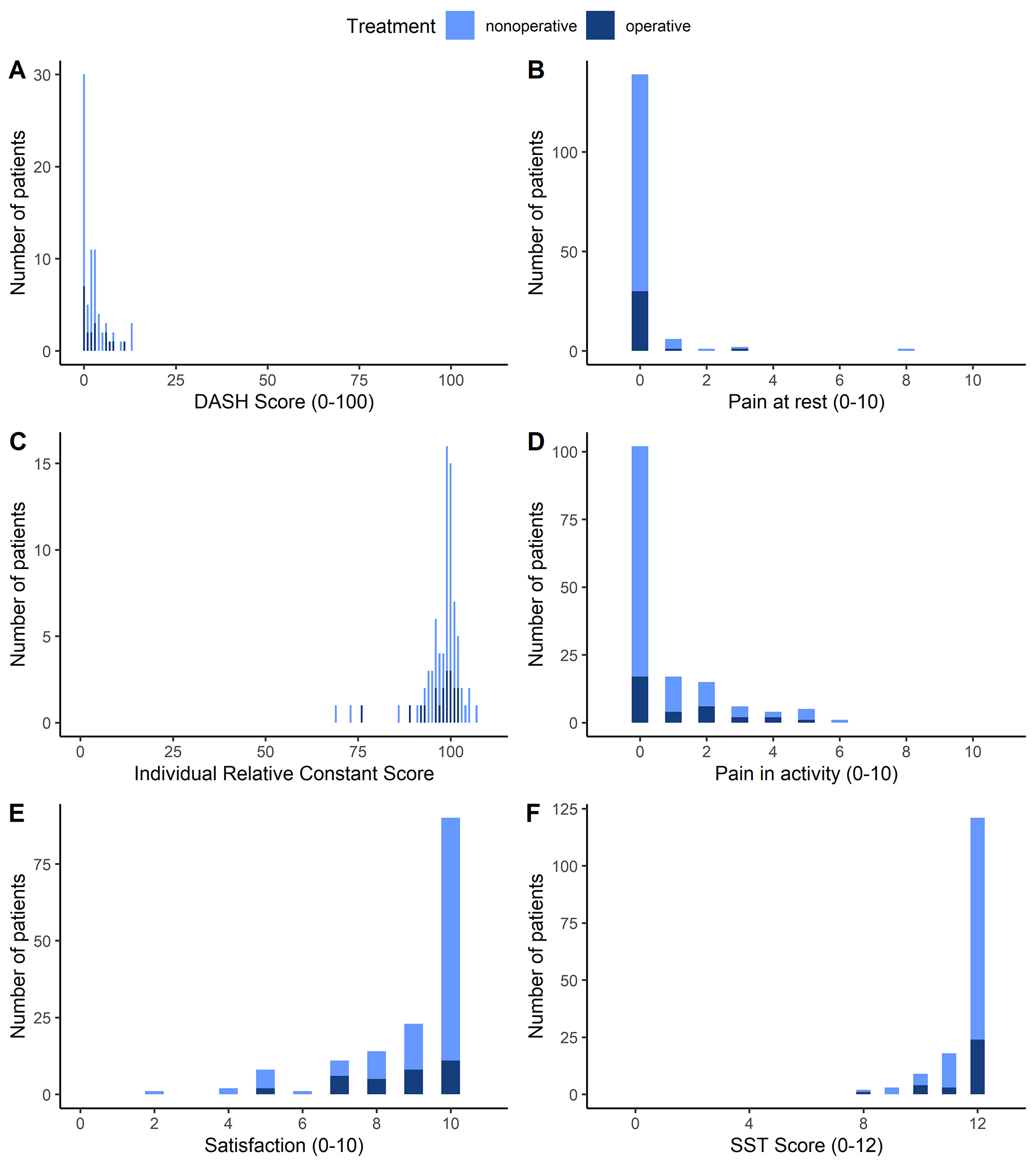
In terms of study details, outcome data were available for 152 patients (153 fractures); 121 fractures had been treated non-surgically, and 32 fractures were treated surgically. Seventy-eight of the patients attended the follow-up visit. Telephone interviews were conducted for the remaining patients.
At follow-up, the mean DASH score (primary outcome) was 2.5. Among the secondary outcomes, a mean score of 11.7 was found for the Simple Shoulder Test (SST). The authors report that DASH, SST, and 15D quality-of-life scores demonstrated no impairment when compared with age-matched normal values. In a propensity-matching analysis, outcomes did not differ between operative and nonoperative treatment.
Reflecting on the study, the message is that this is a fracture that can be treated non-surgically except with massive displacement in older adolescents/young adults. It is our hope that we see more longer-term studies such as this one reporting on the results of other physeal fractures in children and adolescents to help guide us in treatment decision-making.
Read the full study: Outcomes at a Mean of 13 Years After Proximal Humeral Fracture During Adolescence
Additional perspective on this study is offered by Pablo Castañeda, MD in a related commentary article: Sometimes Less Is More!
An Author Insights video is also available with this study at JBJS.org.
JBJS Editor-in-Chief