In this post, JBJS Deputy Editor for Social Media Dr. Matt Schmitz discusses a new study reporting 10-year outcomes of second-generation, all-inside meniscal repair with concomitant anterior cruciate ligament (ACL) reconstruction.
Meniscal repair is a vital part of knee preservation in orthopaedic surgery. Commonly used in conjunction with injuries to the ACL, meniscal repair options have advanced over the years with improvements in instrumentation. Second-generation arthroscopic meniscal repair devices were developed to help improve on some of the problems seen with early devices (chondral injury, mainly).
There are few long-term studies on the rates of healing with these devices. In the June 21, 2023 issue of JBJS, Wright et al. review the long-term clinical results of meniscal repair using a second-generation, all-inside repair device with concomitant ACL reconstruction. Patients had a minimum of 10 years of follow-up.
The investigators identified 81 patients who previously had been enrolled in a prospective database and who had undergone meniscal repair (59 medial, 22 lateral) in conjunction with primary ACL reconstruction between 2002 and 2008. The patients were contacted at 10 years for follow-up. Clinical outcomes were assessed with the International Knee Documentation Committee (IKDC) score, Knee injury and Osteoarthritis Outcome Score (KOOS), and Marx Activity Rating Scale, with both baseline (time of index procedure) and 10-year data available. Clinical failure was defined as a reoperation involving resection or revision repair of the meniscus.
The investigators obtained follow-up data for 69 (85%) of the 81 patients at an average of 10.5 ± 0.4 years (range, 10.0 to 12.5 years). They found that:
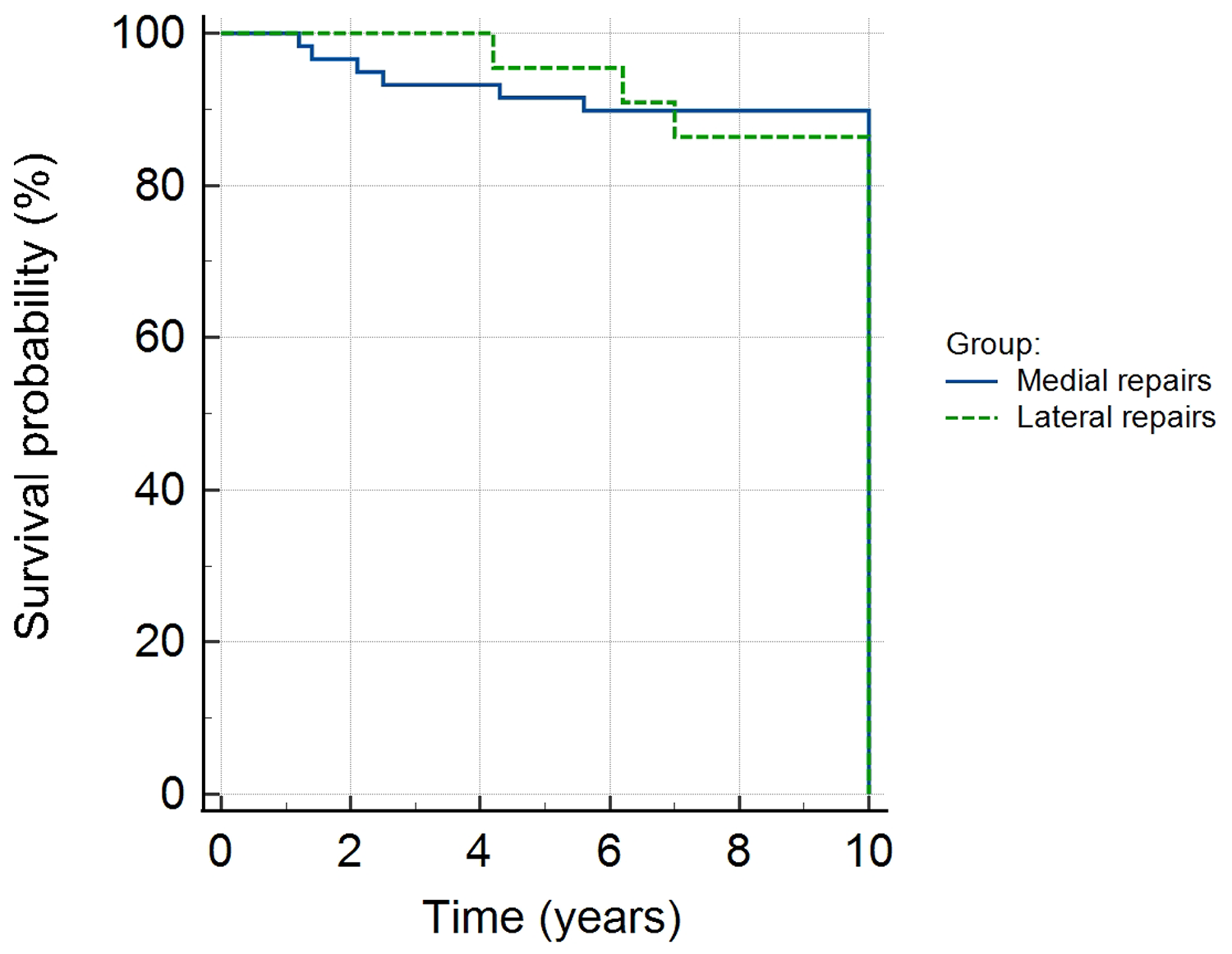
- 9 of 69 experienced failure of meniscal repair (6 medial and 3 lateral), for a 13% failure rate overall
- 6 of 50 medial meniscal repairs failed (12%)
- 3 of 19 lateral meniscal repairs failed (16%)
There were no differences between successful and failed repairs in terms of patient characteristics (age, sex, body mass index) or tear patterns (location, type, or number of sutures). However, the mean time to failure differed significantly between medial repairs (2.8 years) and lateral repairs (5.8 years) (p = 0.002). KOOS and IKDC scores were significantly improved at 10-year follow-up compared with baseline. The Marx Activity Rating Scale score went down (worse) at 10 years, as has been shown in previous studies and is expected with aging.
With successful repair demonstrated at 10 years for 84% to 88% of the patients, this study shows sustainable rates of repair. Long-term data on surgical procedures are important for us to review, especially when we utilize emerging techniques. The old orthopaedic adage of “nothing ruins results like long-term follow-up” may not necessarily be true with second-generation, all-inside meniscal repair performed in the setting of ACL reconstruction.
Additional perspective on this study is provided by Elizabeth Matzkin, MD in a related commentary article: Save the Meniscus: The Meniscal Mantra Remains Durable
See also the related Wolters Kluwer press release: ‘All-inside’ meniscal repair shows good long-term outcomes
Read the full study at JBJS.org: Ten-Year Outcomes of Second-Generation, All-Inside Meniscal Repair in the Setting of ACL Reconstruction
JBJS Deputy Editor for Social Media