A new JBJS study presents novel data on gene expression in glenoid cartilage following shoulder instability. JBJS Deputy Editor for Social Media Dr. Matt Schmitz shares this post.
While shoulder instability may contribute to a higher risk of osteoarthritis (OA), our understanding of the biologic changes that occur in the cartilage of the glenohumeral joint following shoulder instability is limited. So point out Aleem et al., who sought to examine the expression of genes in shoulder cartilage after instability and thus shed further light on the relationship between shoulder instability and the development of OA. Their exploratory study is now published in JBJS:
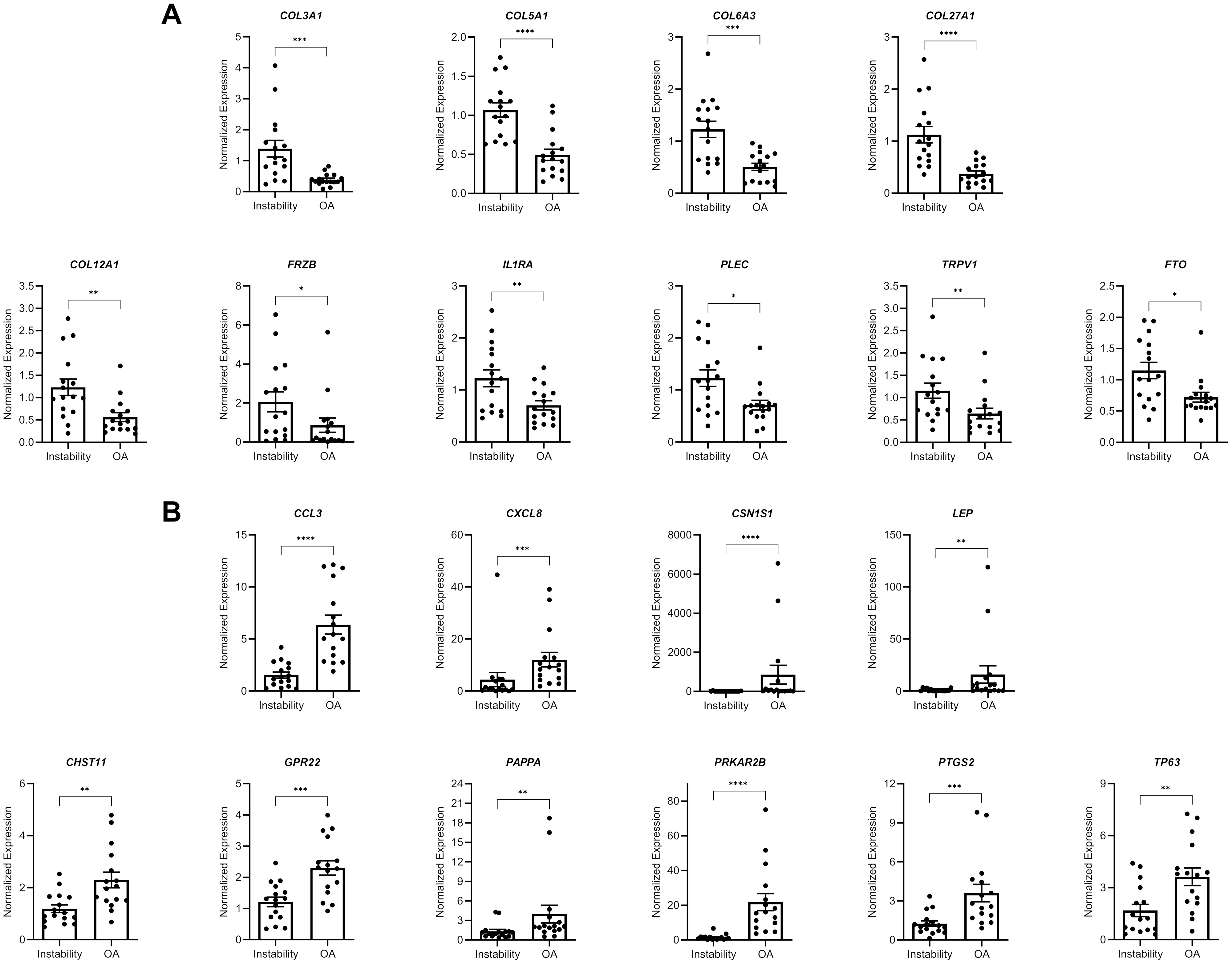
The authors collected glenoid cartilage from 17 patients undergoing stabilization surgery and 16 patients undergoing shoulder arthroplasty for OA. Utilizing quantitative polymerase chain reaction (PCR), they studied the expression of 57 genes, including 36 from OA risk allele studies and 21 from differential expression studies. In comparing gene expression between OA and instability (both chronic [≥3 dislocations] and acute [<3 dislocations]) the authors found the following differences:
Articular cartilage from shoulders with OA undergoing arthroplasty had higher levels of inflammatory and catabolic genes compared with cartilage from shoulders undergoing stabilization surgery, which expressed higher levels of anabolic genes. The findings suggest that certain genes might be important in the development of glenohumeral OA, including CCL3, CHST11, GPR22, PRKAR2B, and PTGS2, which all were higher in the shoulders with OA compared with those with instability.
CCL3 is a pro-inflammatory chemokine that has been linked to OA in other joints and chondral degeneration. The authors note that, interestingly, it was higher in the acute instability group than in the chronic instability group, but higher in the shoulders with OA than either of the instability groups. Another gene expressed predominantly in the OA group was CXCL8, which has also been shown in synovial fluid of arthritic knees and may stimulate the degenerative process of OA. These and other observations of inflammatory and catabolic activity suggest that OA development in the shoulder may be similar to the disease etiology of OA in other joints. The authors further note that genes related to connective tissue extracellular matrix and anabolism were more highly expressed in the instability group, which could suggest a repair response seen in instability as opposed to cartilage degeneration in OA.
The findings of differential gene expression open the door for further research and perhaps the possibility for gene modulation to alter or prevent OA down the road. It doesn’t seem too far-fetched to think of that as attainable given the marked improvements in genetic research and potential therapeutic interventions that could arise from this field of study.
Access the full study at JBJS.org: Gene Expression in Glenoid Articular Cartilage Varies Across Acute Instability, Chronic Instability, and Osteoarthritis
Additional perspective on this study is offered by Dean Wang, MD and Tyler R. Johnston, MD in a related commentary: The Enigma of Posttraumatic Osteoarthritis
JBJS Deputy Editor for Social Media