A new study evaluates sociodemographic factors impacting racial and ethnic disparities in baseline PROM scores of foot and ankle patients. JBJS Editor-in-Chief Dr. Marc Swiontkowski offers this perspective.
In the past 5 years or so, the association of race and ethnicity to health-related outcomes has been more carefully studied than in the history of medicine as we seek to better understand and mitigate disparities in care. What is the interplay of sociodemographic factors? Many issues of poor health, such as hypertension, type 2 diabetes, and cardiac risk, have been clarified to be mostly related to lower income, which in turn, impacts such areas of health as food choice options and access to outdoor and indoor facilities for recreation and play. Moreover, lower income is directly related to education level, impacting access to higher-paying employment. These issues are very tightly linked to self-reported functional measures. A deeper understanding of the factors that influence patient-reported outcome scores will be helpful to addressing racial and ethnic disparities.
Boakye et al. present important clarifying research regarding a cohort of >23,000 patients with foot and ankle conditions who completed the PROMIS (Patient-Reported Outcomes Measurement Information System) tool. A series of statistical models was used to identify the impact of various factors on the health-related functional measures. The study is now published at JBJS.org:
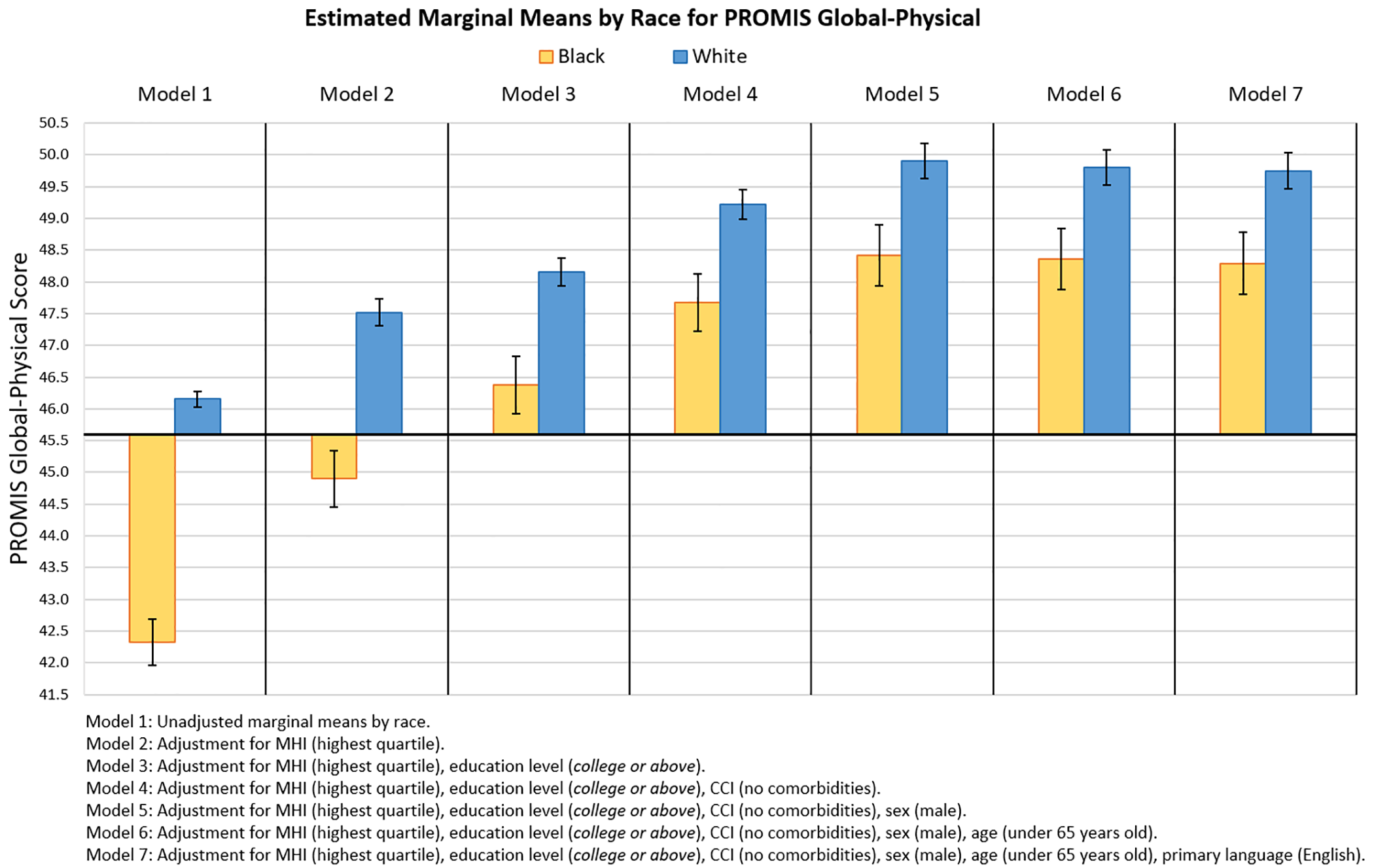
To summarize briefly, the authors retrospectively reviewed baseline PROMIS Global-Physical (PGP) and Global-Mental (PGM) scores. Stepwise regression models were employed to evaluate scores by race and ethnicity after adjusting for household income, education level, primary language, Charlson Comorbidity Index (CCI), sex, and age.
Note the authors, their analyses of the impact of factors on observed racial and ethnic disparities in scores “focused on Black and Hispanic patients, as these groups constituted the largest minority populations in our cohort and were found to experience the largest disparities among the minority populations that we had sufficient numbers to analyze.”
The investigators found that unadjusted mean PGP and PGM scores were 3.8 and 3.9 points lower, respectively, for Black patients than for White patients. The unadjusted mean PGP and PGM scores were 3.3 and 3.4 points lower, respectively, for Hispanic patients than for non-Hispanic patients.
When adjusting for income, education level, and CCI, they found that the racial disparity was reduced by 61% for the PGP and 54% for the PGM. Adjusting for education level, language, and income reduced ethnic disparity by 67% for the PGP and 65% for the PGM.
In the full models, an education level of high school or less and a severe CCI had the largest negative effects on outcome scores. Read the full report by Boakye et al.
As we physicians, nurses, PAs, OTs, and PTs desire to improve the health and functional outcomes of our patients in our day-to-day work lives, we are also required to consider and take appropriate action to help address disparities in care. The data from this cross-sectional study suggest that interventions addressing financial, educational, and language disparities could be appropriate targets to help in this effort. The “ripple effect” of such endeavors, for example, measures to improve access to quality education and thus impact income, may bring meaningful improvement to the health of our communities.
Additional perspective on this study is provided by Alastair S. Younger, MB ChB, ChM, MSc, FRCSC in a related commentary article: Education and Comorbidities Underlie Low Preoperative Scores
An Author Insights video is also available at JBJS.org.
JBJS Editor-in-Chief