When and how would primary care physicians (PCPs) like to hear from orthopaedic surgeons regarding mutual patients? JBJS Deputy Editor for Social Media Matt Schmitz discusses a new study that explores that question.
Being able to efficiently and effectively communicate with referring primary care physicians (PCPs) can have a positive impact on a surgeon’s practice. However, overcommunication can lead to PCPs feeling bombarded and thus may contribute to burnout.
Researchers from Brigham and Women’s Hospital in Boston sought to assess the optimal form and timing of communication from orthopaedic surgeons by asking PCPs directly. The study by Chiodo et al. is now available at JBJS.org. A downloadable infographic accompanies the article:
Primary Care Physician Preferences Regarding Communication from Orthopaedic Surgeons
Surveying 175 PCPs within an academic health network, all of whom used the same electronic medical record system (Epic), the researchers sought to determine:
- Satisfaction with the frequency and quality of patient-related communication from orthopaedists,
- The overall interest in communication from orthopaedists, and
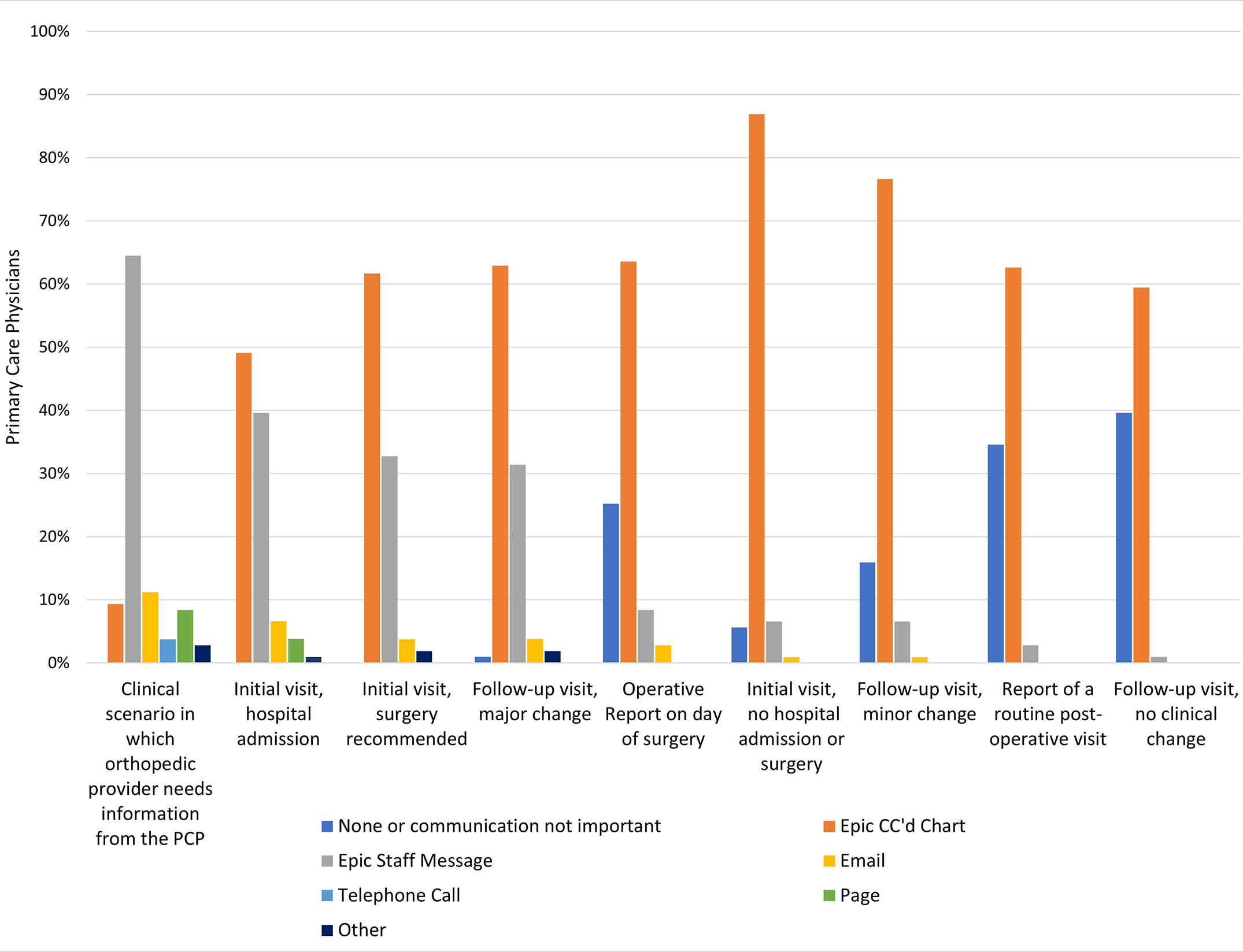
- The perceived importance and preferred method of communication in 9 clinical scenarios (with communication methods including phone call, Epic CC’d Chart, Epic Staff Message, email, pager, fax, none, and other).
- Demographic data were also assessed.
A total of 107 (61.1%) of the PCPs replied to the survey. A majority (60.4%) were female, and most respondents (78.5%) had ≥11 years in practice. In terms of the number of empaneled patients, 27% of respondents had a roster of 500 to 999 patients and another 27%, 1,000 to 1,499 patients; 23% had <500 patients, and 22%, ≥1,500 patients.
With regard to clinical scenarios, the PCPs rated 4 of the 9 as important or very important (“top-box” score of 4 or 5 on a 5-point Likert scale):
- A clinical scenario in which the orthopaedist needs information from the PCP (94.4%; p < 0.001).
- New orthopaedic evaluation requiring immediate hospital admission (92.5%; p < 0.001).
- Initial orthopaedic evaluation with recommendation for surgery (83.2%; p < 0.001).
- Follow-up orthopaedic visit with a major change in clinical status (76.4%; p < 0.001)
For the remaining scenarios—routine initial orthopaedic visit, follow-up visit with minor change or no change, operative report on the day of surgery, and report of a routine postoperative visit—less than half of those surveyed responded that the scenario was important or very important in terms of communication from orthopaedists.
With regard to the preferred method of communication, use of the Epic CC’d Chart was most frequently preferred by PCPs, with the notable exception of when the orthopaedic surgeon needed information from the PCP. In that scenario, PCPs overwhelmingly preferred use of an Epic Staff Message.
The findings of this study suggest that our PCP colleagues do not necessarily want to know everything that we are doing for our mutual patients. Routine follow-up visits or those involving minor changes likely don’t require us to send messages to the PCP. Future studies could elucidate whether cutting down on some communication deemed unnecessary might help with perceived burnout.
It was interesting that, in this study, 25% of PCPs reported spending >3 hours in the electronic medical record after their clinical activities were over for the day, and nearly 87% spent 1 to 1.5 hours after their normal clinical hours. By being more efficient in our communication and using pointed messages through avenues that certain electronic medical records allow, we can hopefully help alleviate to some degree the increased burden of “computer clicks” for our colleagues in primary care. Whether that impacts time in the medical record and thus improves burnout needs to be studied for all of us as physicians.
Read the full report: Primary Care Physician Preferences Regarding Communication from Orthopaedic Surgeons
JBJS Deputy Editor for Social Media