Early in my orthopaedic residency training, I remember an attending surgeon quizzing me on the mortality rate for elderly patients who sustained a hip fracture. Studies suggest that approximately 10% to 30% of elderly patients may die within one year following a hip fracture. Factors influencing mortality include age, overall health, the presence of comorbidities, and the type of surgical intervention received. The concern is not just the hip fracture itself, but what the fracture may also represent in terms of the overall physical decline of the patient.
Earlier this month in JBJS, a study by Mundi et al. from Canada found that patients who experienced a periprosthetic joint infection (PJI) in the first year after total hip arthroplasty (THA) had a fivefold increased risk of mortality within 10 years compared with matched patients without PJI. In an accompanying editorial, JBJS Editor-in-Chief, Dr. Mo Bhandari states that the study “helps to shed light on the devastating complication of PJI following joint replacement surgery—and serves as a call to action to researchers to design, execute, and disseminate high-quality studies on PJI prevention and treatment.”
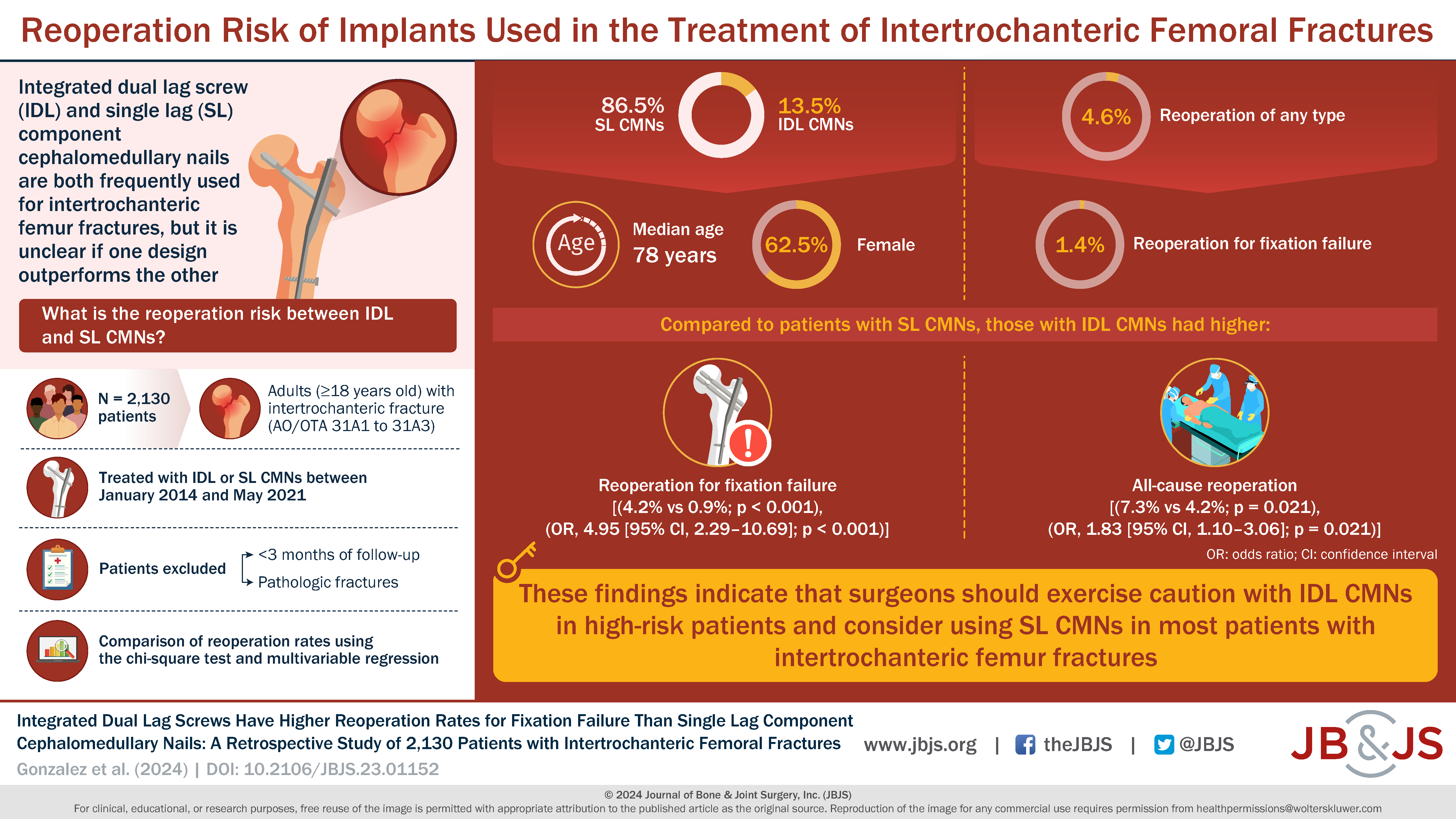
In the new issue of JBJS, Gonzalez et al. with the Hip Fracture Nail Study Group present the results of a retrospective study comparing reoperation rates for fixation failure in patients with an intertrochanteric femoral fracture treated with either an integrated dual lag screw (IDL) or single lag component (SL) cephalomedullary nail (CMN). The study included 2,130 patients from 13 Level-I trauma centers (median patient age, 78 years; 62.5% female).
The investigators found that patients with IDL CMNs had significantly higher rates of reoperation for fixation failure (4.2% versus 0.9%; p < 0.001) and all-cause reoperation (7.3% versus 4.2%; p = 0.021) compared to those with SL CMNs. After controlling for various factors, IDL CMNs were associated with significantly higher odds of reoperation for fixation failure (4.95 times greater) and all-cause reoperation (1.83 times greater) than SL CMNs.
The authors suggest caution in using IDL CMNs for high-risk patients and recommend SL CMNs for most intertrochanteric femoral fractures. Here’s the link to the study and visual abstract:
It goes without saying that we would want to decrease the rates of reoperation and complications in our potentially most fragile patients. Although Gonzalez et al. did not look specifically at mortality, we know that elderly patients with a hip fracture have a notable mortality risk, so trying to minimize complications, much like minimizing PJI in patients undergoing THA, calls for our vigilance. Older patients with hip problems (fractures, severe arthritis) deserve our continued research efforts to help maximize their surgical outcomes and minimize complications.
JBJS Deputy Editor for Social Media
Related reading on OrthoBuzz:
Periprosthetic Joint Infection After Hip Replacement Linked to Increased Mortality
Interested in more hip content? Check out What’s Trending? at JBJS.org.