Dr. Matt Schmitz, JBJS Deputy Editor for Social Media, discusses 3 recent studies that reflect the rigorous standards, and challenges, of randomized clinical trials (RCTs).
Randomized clinical trials (RCTs) are the holy grail in research. When done correctly, they represent the highest levels of evidence in scientific methodology and sit at the top of the hierarchy of peer-reviewed clinical research.
However, as anyone who has been involved in scientific research can tell you, RCTs are often incredibly difficult to perform. They are costly, may necessitate coordination among multiple research centers, and can be a headache logistically. They require gaining approval by ethics boards and recruiting patients who agree to randomization. All of these potential obstacles compound to make completing these studies difficult—in the hopes of answering important questions in musculoskeletal care.
Three multicenter RCTs are among studies featured in the January issues of JBJS:
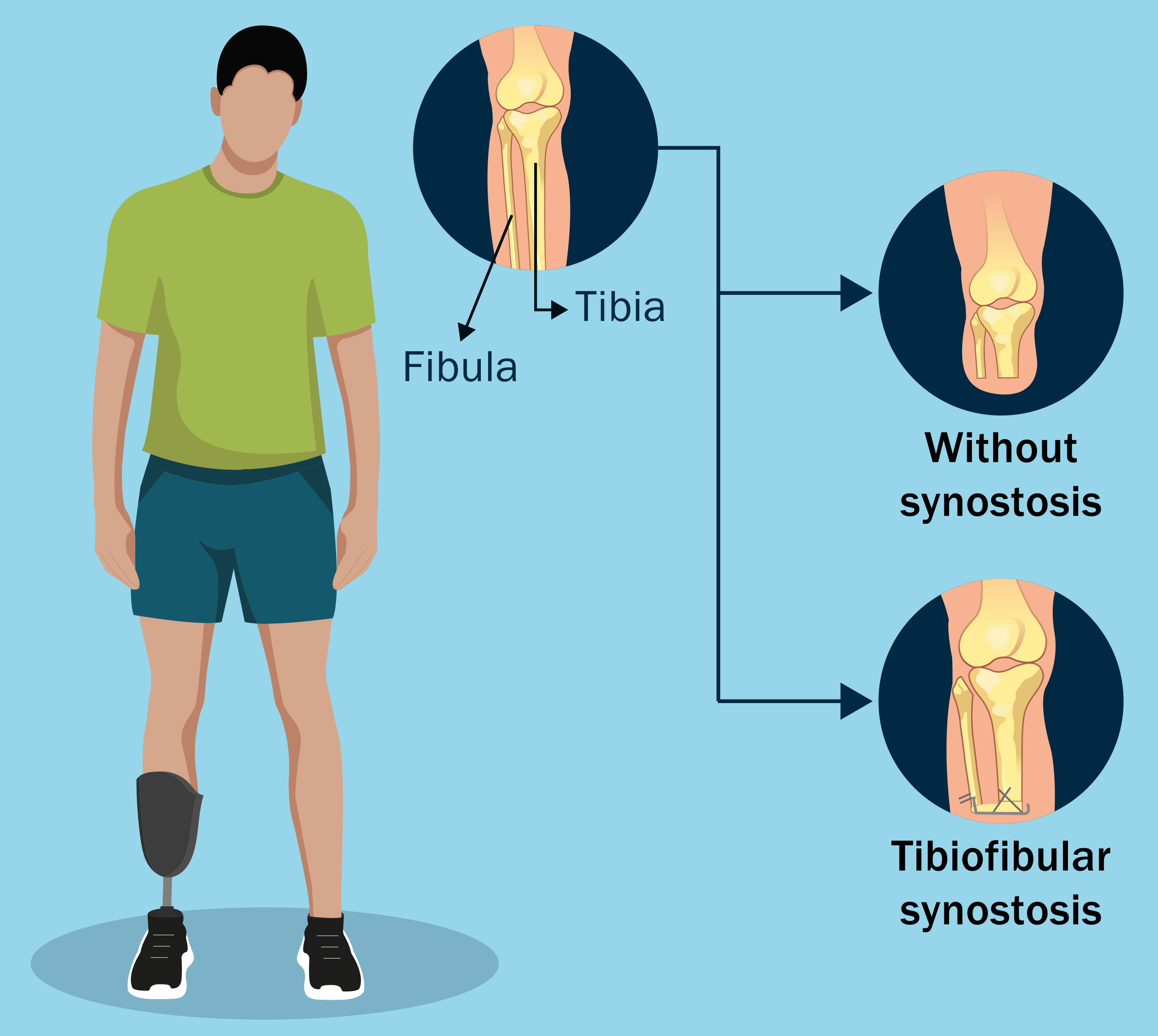
Outcomes Following Transtibial Amputation with and without a Tibiofibular Synostosis Procedure. A Multicenter Randomized Clinical Trial (TAOS Study)
In a study conducted by the Major Extremity Trauma Research Consortium (METRC), researchers compared outcomes of patients undergoing transtibial amputation with (54 patients) or without (52 patients) a tibiofibular synostosis procedure. Included were patients 18 to 60 years of age. There were also 93 participants (31 synostosis, 62 non-synostosis) who opted out of randomization and were enrolled in an observational study. Download the visual abstract of this study.
The primary outcomes were operative treatment for a complication within 18 months and scores of the Short Musculoskeletal Function Assessment (SMFA). Data from the observational cohort were included in secondary analysis to enhance the robustness of the findings.
Findings: The investigators found that the synostosis group had a higher probability of ≥1 operatively treated complication (42% compared to 24% for the non-synostosis group; absolute risk difference: 18%). No significant differences between the groups in terms of mean SMFA scores were observed in the primary analysis. In the secondary analysis, the synostosis procedure still was linked to a higher probability of an operatively treated complication (absolute risk difference: 26.1%), and while SMFA scores showed some advantages for synostosis, differences in pain, prosthetic use, and satisfaction remained statistically nonsignificant.
As with many RCTs, there were limitations, one of which was not meeting the target enrollment. A notable crossover rate in treatment assignments also was observed, although the authors note that they found no difference in the results of their intention-to-treat and as-treated analyses. Overall, the study provides valuable insights into complications and functional outcomes associated with tibiofibular synostosis during transtibial amputations.
Open-Door Cervical Laminoplasty Using Instrumentation of Every Level Versus Alternate Levels. A Multicenter, Randomized Controlled Trial
Another multicenter RCT, performed by Tamai et al. in Japan, investigated the effectiveness of skip- versus all-fixation methods in open-door cervical laminoplasty for treating degenerative cervical myelopathy. The researchers aimed to assess the noninferiority of skip-fixation (instrumentation of every second opened level) and evaluate various surgical and radiographic outcomes. Access the Author Insights video for this study.
Included were patients ≥60 years undergoing C3 to C6 laminoplasty. Participants were randomly assigned to either skip-fixation (n = 80) or all-fixation (n = 75).
Of the 155 randomized patients,130 completed the study (83.9% follow-up rate). The difference in the Japanese Orthopaedic Association (JOA) score at 2 years postoperatively, the primary outcome, was 0.0298 (95% CI, –0.706 to 0.766), confirming noninferiority of skip-fixation (p < 0.0001). Secondary analyses revealed that skip-fixation resulted in significantly shorter mean surgical time (106.0 vs. 117.6 minutes; p = 0.010) and greater improvement in the VAS for neck pain, the Neck Disability Index, and quality of life as measured by the EQ-5D-5L. No significant differences were observed in radiographic outcomes or complications.
Conclusions: The authors concluded that skip-fixation during open-door cervical laminoplasty may be sufficient to achieve comparable improvement in myelopathy at 2 years, with additional benefits in terms of surgical time and recovery metrics such as neck pain and quality of life. The findings suggest that selecting skip-fixation could simplify the procedure without compromising patient outcomes. This investigation opens the door for longer-term studies to further assess the noninferiority of skip-fixation.
Multicenter Randomized Clinical Trial of Highly Cross-Linked Polyethylene Versus Conventional Polyethylene in 518 Primary TKAs at 10 Years
Finally, Salmons et al. performed an RCT at 3 Mayo Clinic locations to assess the long-term outcomes of highly cross-linked polyethylene (HXLPE) compared to conventional ultra-high molecular weight polyethylene (UHMWPE) in primary total knee arthroplasty (TKA). Enrolled in the study were 518 patients with a mean age at TKA of 67 years and a mean body mass index of 32 kg/m²; 58% of the patients were female. The randomization process ensured blinding; 254 knees (control group) received a UHMWPE insert and 264 knees received an HXLPE insert. Both groups underwent the same surgical procedure: cemented posterior-stabilized TKA with patellar resurfacing. The mean follow-up was 11 years for the 383 patients who were alive and revision-free at 10 years. Download the visual abstract of this study.
The investigators found that the 10-year survivorship free from revision (the primary outcome) was 96% overall, 97% for the HXLPE group, and 96% for the UHMWPE group. Survivorship free from any reoperation was 94% overall, 96% for the HXLPE group, and 92% for the UHMWPE group. The risk of revision or reoperation did not differ significantly between the groups.
Both groups showed significant improvement in Knee Society Score (KSS) values and the SF-12 Physical Component Summary from preoperatively to the 10-year mark, with no significant differences between the groups. There were 19 revisions, with no revision due to wear, osteolysis, or fracture in the HCLPE group, but 1 case of osteolysis-associated fracture in the UHMWPE group. The results of radiographic evaluation were otherwise similar between the groups, including no evidence of loosening and minimal nonprogressive radiolucent lines observed.
Conclusions: The authors concluded that both HXLPE and UHMWPE inserts demonstrated excellent long-term performance in primary cemented TKA. The absence of wear-related failure in the HXLPE group suggests it could be a preferable choice for knee arthroplasty, especially considering its comparable survivorship and clinical outcomes relative to UHMWPE.
The study’s acknowledged limitations include the potential for bias given that 14% of the patients were lost to follow-up, and the need for longer-term data to fully assess wear-related failure. The authors also note that the findings may not apply to other implant designs or newer cementless techniques.
For additional perspective on this study, see the related commentary by Jeremy M. Gililland, MD: Compelling Evidence Regarding Long-Term Performance of Highly Cross-Linked Versus Conventional Polyethylene in TKA at 10 Years.
I commend the authors of these studies for doing the hard work of an RCT. While all of the studies have limitations that are inherent and perhaps unavoidable in even the best-planned RCTs, they help to answer some important questions and bring forth considerations for future research efforts.
Orthopaedic surgery has come a long way since the “This is how I do it” phase of research. I look forward to other high-level RCTs on the pages of JBJS in the near future.
JBJS Deputy Editor for Social Media