In this post, Dr. Matt Schmitz, JBJS Deputy Editor for Social Media, spotlights 3 total joint arthroplasty studies featured in the February 19, 2025 issue of JBJS.
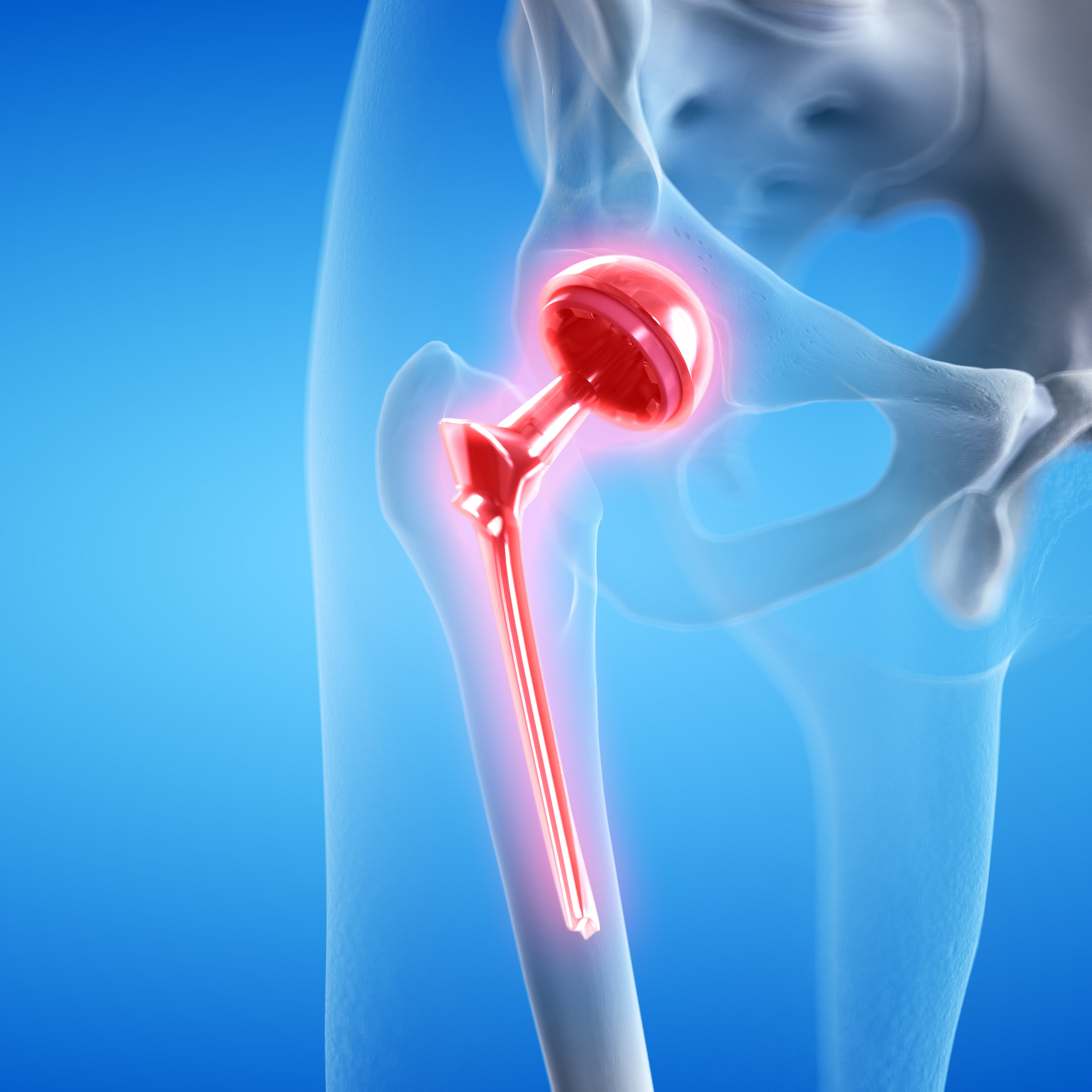
Total joint arthroplasty (TJA) is a common procedure for many orthopaedic surgeons and a successful treatment strategy for reducing pain and improving function in our patients. Researchers continue to extensively study ways to decrease complications, lengthen the survivability of implants, and optimize patient outcomes. In the latest issue of JBJS, 3 studies provide valuable insights into total hip and knee arthroplasty:
Glucagon-Like Peptide-1 Receptor Agonists Decrease Medical and Surgical Complications in Morbidly Obese Patients Undergoing Primary TKA
Kim et al., from the Hospital for Special Surgery in New York, evaluated the impact of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) on surgical and medical complications in patients with morbid obesity (BMI of ≥40 kg/m²) undergoing primary total knee arthroplasty (TKA). Using an administrative claims database, 2 cohorts were analyzed: patients taking GLP-1 RAs pre- and post-surgery and a control group not using these medications.
The investigators found significant reductions in the rates of 90-day complications, including periprosthetic joint infection (PJI), medical complications, and readmission, for those taking GLP-1 RAs compared with the control group. Rates of 2-year surgical complications did not differ. In addition, the reduced complication rate in the GLP-1 RA group was similar to that of patients with severe obesity (BMI of 35.0 to 39.9 kg/m²) undergoing TKA.
The authors note the need for randomized clinical trials to clarify the effectiveness of GLP-1 RAs in optimizing outcomes for patients with obesity undergoing TKA, but the early results look promising for these medications, which are becoming commonplace in the U.S. Read the study and access the visual abstract.
More perspective on this study is shared by Donald W. Roberts in a commentary article: Total Knee Arthroplasty and Morbid Obesity: Is There a Glimmer of Hope?
Outcomes Following Direct Anterior Approach Total Hip Arthroplasty: A Contemporary Multicenter Study
In a study conducted at the Mayo Clinic, Wilson et al. investigated the outcomes of 3,698 primary total hip arthroplasties (THAs) performed using the direct anterior approach, from 2010 to 2019 across 3 institutions within their health-care system. Patients had an average age of 65 years and an average BMI of 29 kg/m².
At 10 years, revision-free survivorship was 96% and reoperation-free survivorship was 94%. The leading indications for revision were PJI, periprosthetic fracture, and aseptic loosening. Notably, a BMI of ≥40 kg/m² was significantly associated with increased risk of PJI and reoperation. The study also found a low incidence of instability-related revision, at just 0.14% at 5 years.
Overall, the authors concluded that THA with the direct anterior approach had satisfactory survivorship at early to intermediate follow-up. However, they advise caution for patients with high BMI due to higher complication rates. Read the study and access the video abstract.
Further commentary is provided by Friedrich Boettner, MD: Not a One-Size-Fits-All Approach for Total Hip Arthroplasty?
Perioperative Geriatrician Assessment Is Associated with a Lower Risk of Emergency Department Visits After Total Joint Arthroplasty
In a study performed at Brigham and Women’s Hospital in Boston, Liimakka et al. investigated the impact of perioperative geriatrician assessments on outcomes for elderly patients undergoing elective TJA. Analyzing the data of 16,076 patients ≥65 years of age, the researchers found that geriatrician visits, particularly within 1 week prior to surgery, were associated with significantly lower odds of postoperative emergency department visits (odds ratio [OR], 0.97; 95% confidence interval [CI], 0.68 to 0.99; p = 0.005]. This effect was most notable for patients 65 years of age (OR, 0.66 [95% CI, 0.45 to 0.98]).
The findings suggest that geriatrician involvement may enhance postoperative care, potentially reducing morbidity and health-care costs. While no significant difference in length of hospital stay was observed, trends indicated increasing utilization of geriatrician consultations over time. The findings support the potential of integrating geriatricians into the perioperative process to optimize outcomes for elderly patients undergoing TJA and highlight the need for further research to validate these results in diverse health-care settings. Read the study.
Learn more about this study from co-author Adriana Liimakka, MBI in an Author Insights video.
Taken together, these studies highlight new insights into TJA. Whether examining the effect of weight-control pharmaceuticals, surgical approach, or the potential for better coordination with our medical colleagues—it is incumbent upon us as orthopaedic surgeons to seek the best outcomes for those in our care. I look forward to new prospective studies on ways to lower perioperative risks and optimize outcomes for all patients.
JBJS Deputy Editor for Social Media
Also in the new issue of JBJS:
Prospective Noninvasive Hemoglobin Monitoring in the Outpatient Total Joint Arthroplasty Setting