Dr. Matt Schmitz, JBJS Deputy Editor for Social Media, highlights 2 new Level-I studies in total joint arthroplasty.
Total knee arthroplasty (TKA) and total hip arthroplasty (THA) are 2 of the most successful orthopaedic procedures in terms of helping our patients regain function and improve quality of life. Even with their high success rates, it’s worth our effort to continue to seek ways to improve the patient experience with total joint procedures—including in the early postoperative period.
The use of adjunctive medications is one method of improving postoperative pain and other symptoms. But we should be cautious in their use when weighed against their potential to cause deleterious effects following joint replacement. In the May 21, 2025 issue of JBJS, 2 high-quality randomized control trials (RCTs) offer new insights.
The first study, by Park et al., examines the effects of intravenous (IV) dexamethasone on blood glucose levels, insulin requirements, postoperative pain, and postoperative nausea and vomiting (PONV) in patients with well-controlled type-2 diabetes mellitus undergoing TKA.
The study, performed in Seoul, South Korea, involved 83 patients with a preoperative glycated hemoglobin level of ≤7.0%. They were randomized to receive either IV dexamethasone 1 hour prior to TKA and on postoperative day 1 or normal saline solution as a placebo at the same time points.
The researchers found that the administration of IV dexamethasone transiently increased blood glucose levels on the day of surgery and postoperative day 1, with levels returning to baseline by postoperative day 3. They also found that insulin requirements were significantly higher in the dexamethasone group on postoperative day 1.
In terms of pain, however, dexamethasone effectively reduced pain levels up to 3 days postoperatively. The mean numeric rating scale (NRS) for pain at rest was lower in the dexamethasone group compared to the control group up to 6 hours after surgery and on postoperative days 2 and 3 for pain during activity. The investigators did not find any significant differences in PONV between the 2 groups.
The findings of this Level-I study suggest that, while IV dexamethasone increases blood glucose levels and insulin requirements temporarily in diabetic patients undergoing TKA, it may provide notable benefits by reducing early postoperative pain. The authors highlight the importance of considering these effects in the perioperative management of patients with diabetes, although one should note that they only included those with well-controlled diabetes in their study group, so these results should not be extrapolated to patients with poorly controlled diabetes and a potential for increased risk of infection.
A commentary by Elizabeth G. Lieberman, MD provides additional insights into this study: Worth the Hype(rglycemia)? Dexamethasone in Diabetic Patients Undergoing Total Knee Arthroplasty
Adding to the conversation on dexamethasone, Jiang et al. present an RCT investigating the efficacy of vitamin C as a substitute for glucocorticoids (specifically dexamethasone) in reducing pain and inflammation following THA. Conducted at the authors’ institution in the People’s Republic of China, the study involved 107 patients who were randomized to 1 of 3 groups: vitamin C, dexamethasone, or control (neither vitamin C nor dexamethasone).
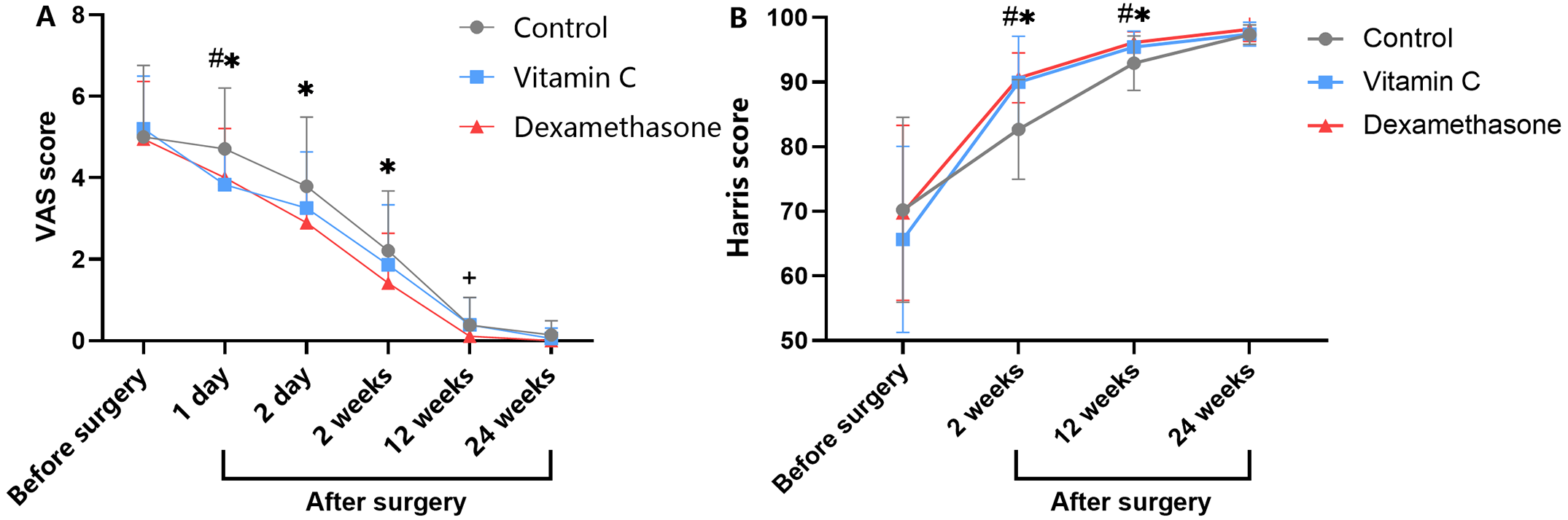
The researchers found that both the vitamin C and dexamethasone groups reported significantly lower pain scores on a visual analogue scale (VAS) on postoperative day 1 compared to the control group. Perioperative morphine consumption was also lower in the treatment groups. Patients receiving either vitamin C or dexamethasone demonstrated lower levels of C-reactive protein as well as lower levels of fibrinogen and higher levels of D-dimer. In addition, Harris hip scores were significantly higher in both the Vitamin C and dexamethasone groups at 2 and 12 weeks post-surgery compared to the control group, showing improved function. Vitamin C did not significantly affect blood glucose levels, unlike dexamethasone, which was associated with greater blood glucose levels after surgery. In this study, both treatment groups had a lower rate of PONV than the control group.
The findings suggest that vitamin C may be a safe and effective alternative to the glucocorticoid dexamethasone for managing pain and inflammation after THA, with the added benefit of not adversely affecting blood glucose levels. The authors advocate for additional research to further explore the mechanisms and long-term effects of vitamin C in postoperative care.
Both of these high-quality Level-I studies show that medical adjuncts can offer some improvements in the postoperative period for patients undergoing total joint arthroplasty. Future studies of Vitamin C and dexamethasone could further examine their interactions with blood glucose and their potential role for patients with diabetes as well as their use more broadly to help improve pain and function in the early postoperative period following joint replacement.
JBJS Deputy Editor for Social Media