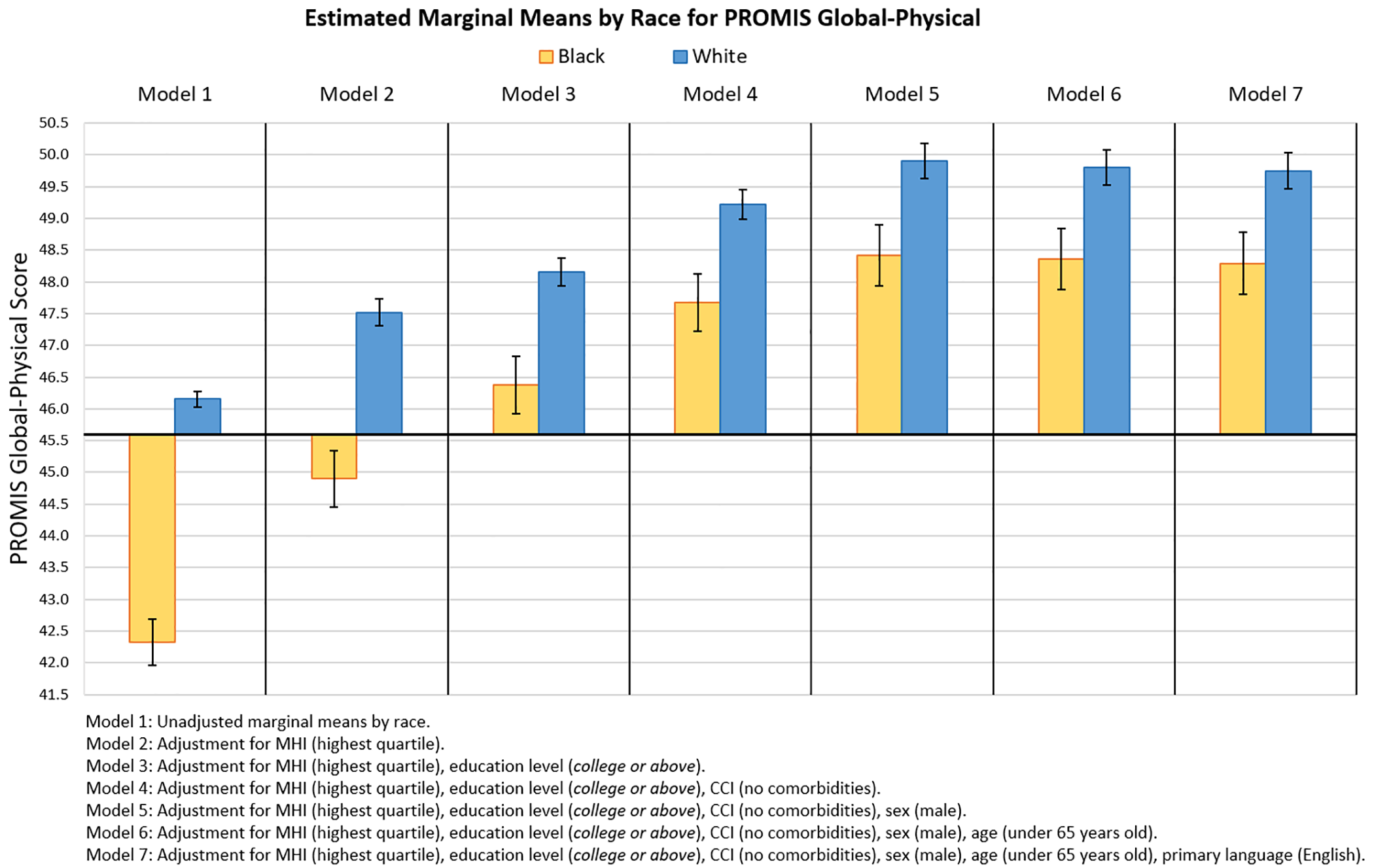
A new study evaluates sociodemographic factors impacting racial and ethnic disparities in baseline PROM scores of foot and ankle patients. JBJS Editor-in-Chief Dr. Marc Swiontkowski
Search Results for: Editor's Choice May 5
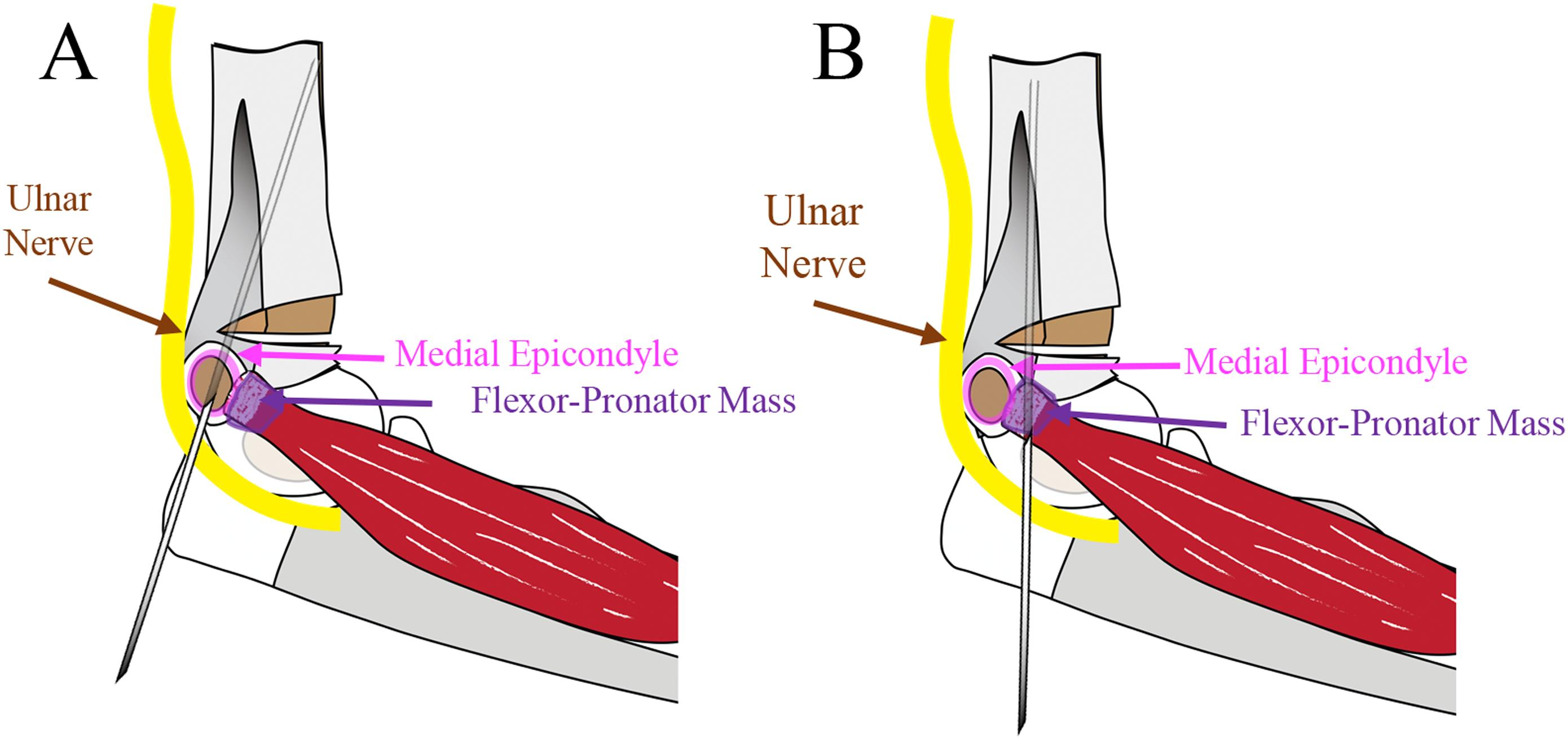
Percutaneous pinning of displaced supracondylar humeral fractures (SCHFs) in children has been the treatment of choice for decades. The debate regarding all-lateral pinning versus cross-pinning
I’ll be honest: I have never worried much about breakage of the cephalomedullary nails I implant for proximal femur fractures. Instead, I’m focused on the
The article “Declining Rates of Osteoporosis Management Following Fragility Fractures in the U.S., 2000 through 2009” by Balasubramanian, et al. in the April 2, 2014