Noteworthy findings regarding topics such as platelet-rich plasma injection, botulinum toxin injection, and microinvasive trigger-finger release, among others, are presented in the new JBJS Guest
Category: What’s New
Recent findings in rotator cuff repair, shoulder arthroplasty, and fracture management are among the topics of interest in the new JBJS Guest Editorial What’s New
Periprosthetic joint infection, venous thromboembolism prevention, and implant cost-utility are among the focuses of the new JBJS Guest Editorial What’s New in Hip Surgery. Here,
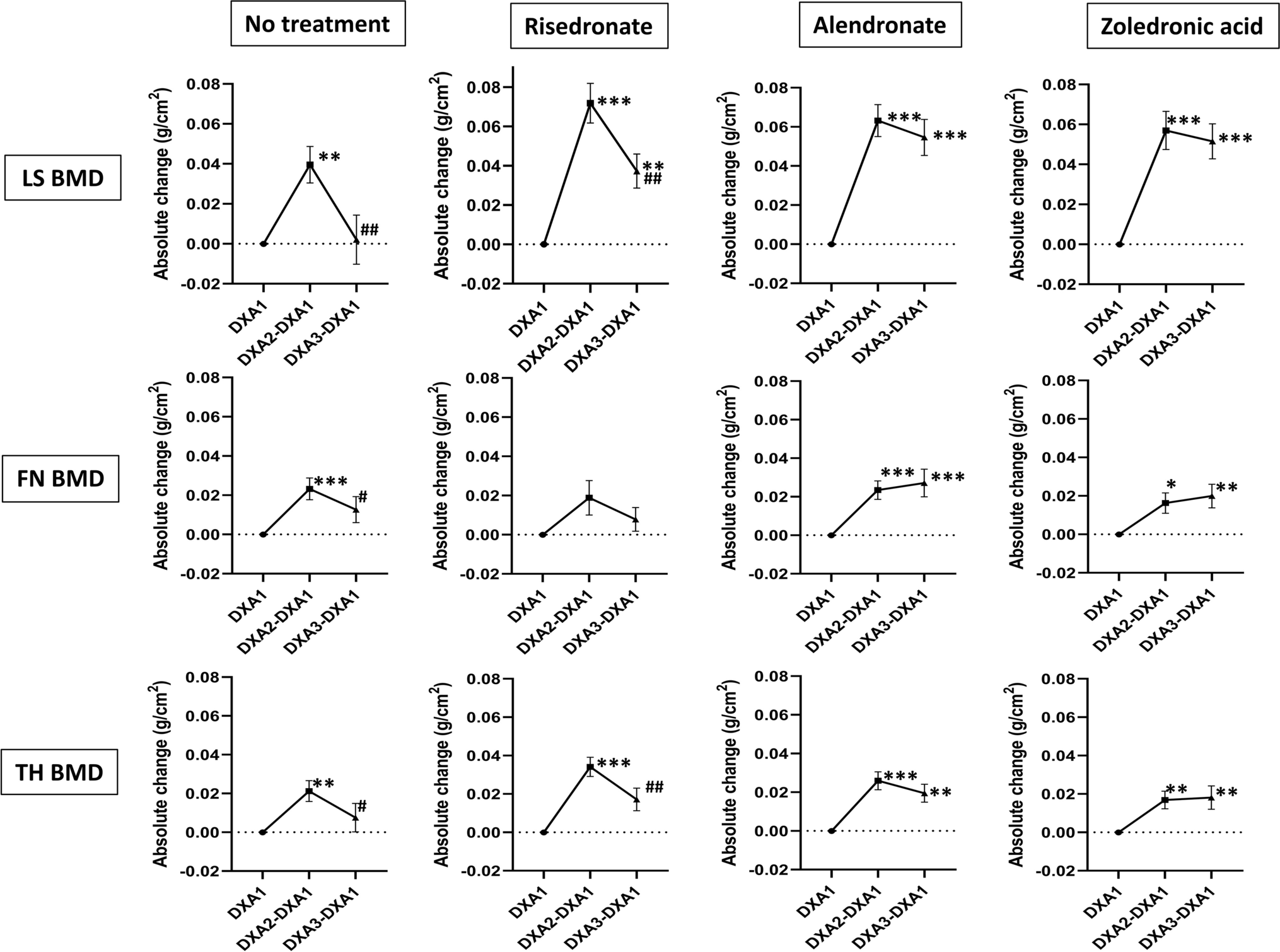
Vitamin D supplementation, fracture risk, and osteoporosis drug therapies are among several topics explored in recent studies featured in the new JBJS Guest Editorial: What’s
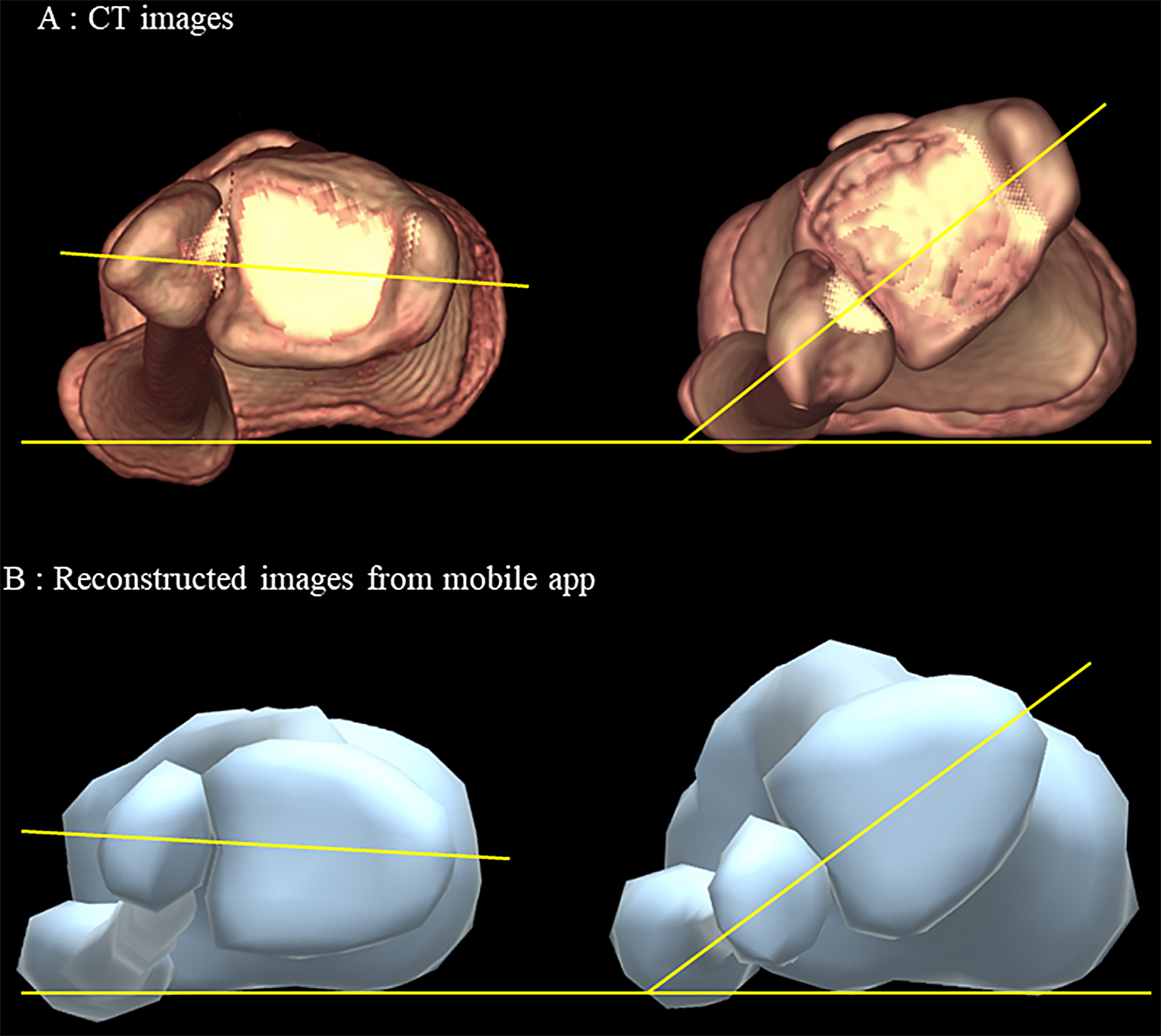
Topics of interest, including a new 3D reconstruction tool for the lower leg, infection rates of pin sites treated with primary closure versus secondary wound
The new JBJS Guest Editorial “What’s New in Musculoskeletal Infection” presents findings related to chronic periprosthetic joint infection, oral antibiotic prophylaxis, and more. Here, we
Recent findings on fracture management and other trauma-related topics are presented in the new JBJS Guest Editorial “What’s New in Orthopaedic Trauma.” Here, we highlight
Recent studies on topics such as rates of lumbar spinal stenosis recurrence and the cost-effectiveness of early microdiscectomy are discussed in the new JBJS Guest

Long-term survivorship of total ankle arthroplasty, rerupture rates associated with the treatment of acute Achilles tendon rupture, and other important findings are presented in the

Topics of interest in the new JBJS Guest Editorial “What’s New in Sports Medicine” include opioid-sparing analgesia, risk of graft failure following meniscal allograft transplantation,

