Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 subspecialties. Click
Month: May 2021
Some years ago, we moved away from calling hip dysplasia “congenital” and started using the term “developmental dysplasia of the hip” (DDH). Indeed, it is
Co-author Ran Schwarzkopf, MD, MSc discusses the new JBJS study “Tranexamic Acid Is Safe in Patients with a History of Coronary Artery Disease Undergoing Total Joint
Terminology is important in orthopaedics. When teaching, for instance, we stress the need for trainees to be able to articulate what a radiograph is showing
OrthoBuzz occasionally receives posts from guest bloggers. In response to a recent article in Ultrasound in Medicine and Biology by Bekhet et al., this commentary
With the increasing effectiveness of immunotherapy and chemotherapy, patients with metastatic disease are surviving longer in much higher numbers. For many primary tumors (lung, breast,
The analysis did not identify evidence that the results of TSA were statistically or clinically improved over the 2 decades of study or that any
In the May 5, 2021 issue of JBJS, Tomizuka et al. report the results of mechanical testing in which they quantified the loss of supination
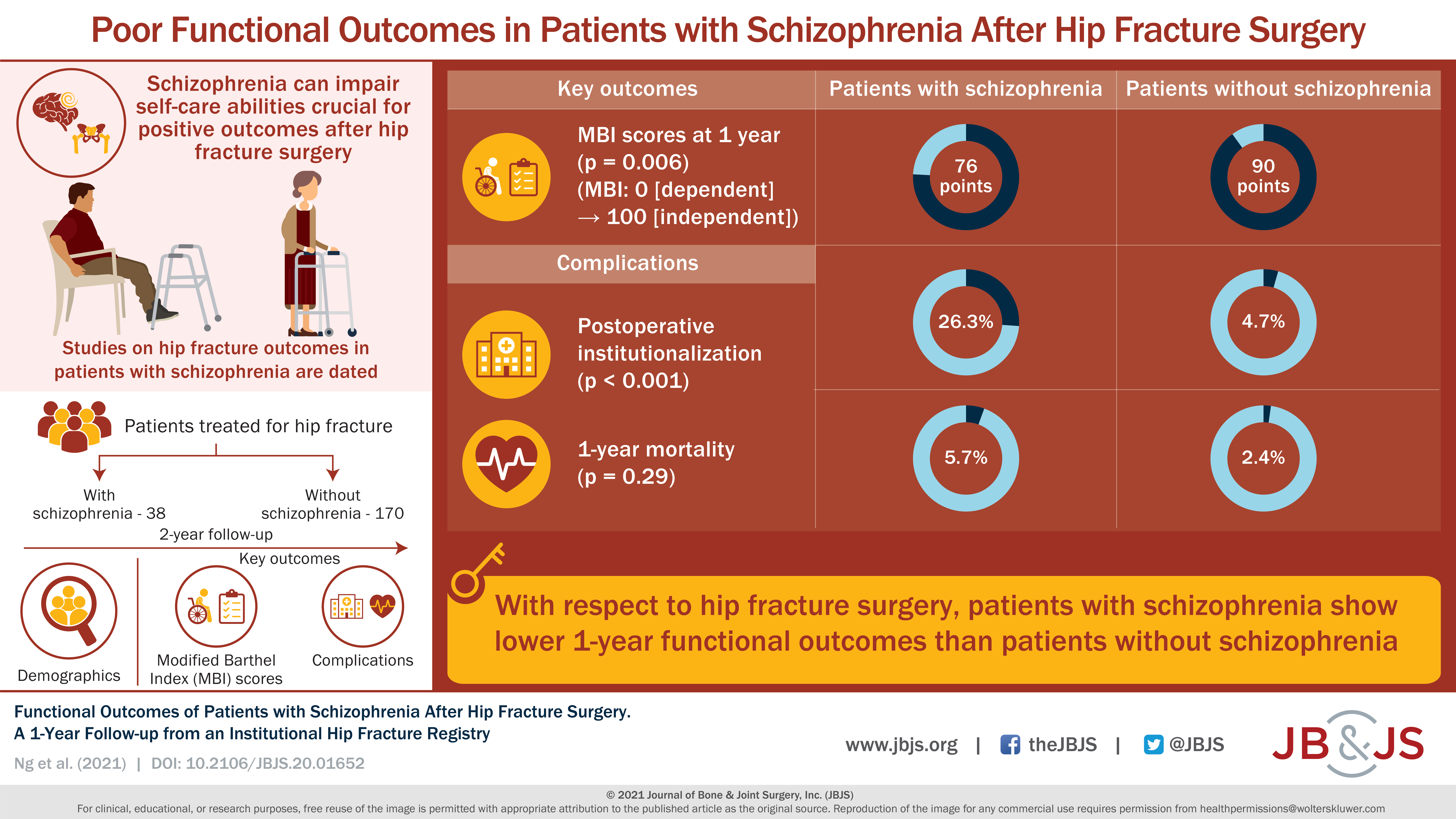
Thirty-eight patients with schizophrenia were compared with 170 geriatric patients without schizophrenia who underwent a surgical procedure for a hip fracture. Read the full article
JBJS Editorial — Podcasts are an increasingly important mode of communication across many segments of society. Our field was perhaps a bit slow to catch
