Every month, JBJS publishes a review of the most pertinent and impactful studies published in the orthopaedic literature during the previous year in 14 subspecialties. Click
Month: July 2021
Genetic susceptibility to orthopaedic conditions is of interest to clinicians and patients alike. While the link between genetics and certain pediatric conditions is known, studies
Co-author Anne R. Bass, MD discusses the new JBJS study “Periprosthetic Joint Infection Is Associated with an Increased Risk of Venous Thromboembolism Following Revision Total Knee
There have been 3 historic cycles of interest in surface replacement of the hip in the last 40 years. The second cycle occurred in the 1980s into the 1990s, when

All recipients of the JBJS Robert Bucholz Journal Club Grant are asked to complete an end-of-year survey that includes a question about how they used
In a study now reported in JBJS, Acuña et al. analyzed Medicare reimbursements associated with revision total hip arthroplasty (THA) procedures. After adjusting for inflation, they found that the mean

Every month, JBJS publishes a review of the most pertinent and impactful studies reported in the orthopaedic literature during the previous year in 14 subspecialties. Click here for a collection of all such OrthoBuzz specialty-update summaries. This
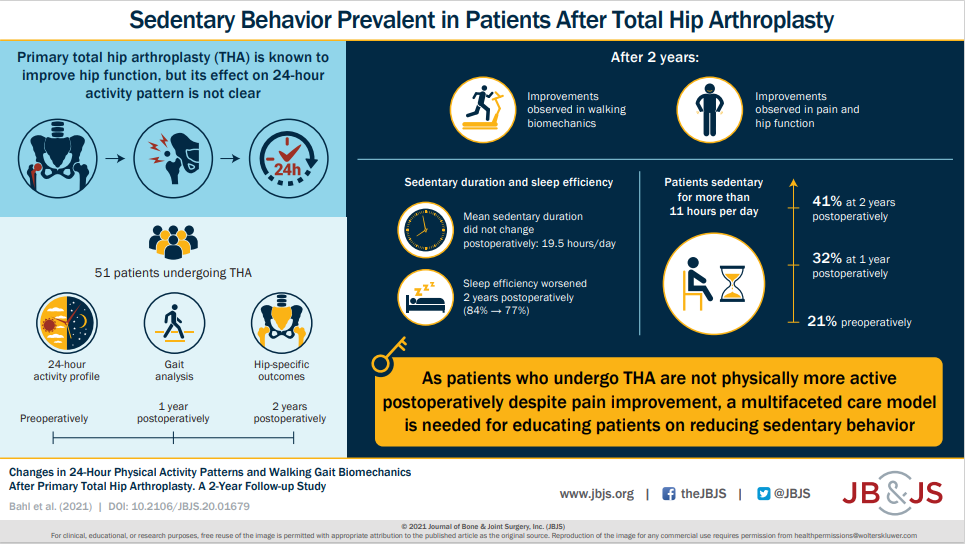
Together with improvements in self-reported pain and perceived physical function, patients had significantly improved gait function postoperatively. Read the full article here.
The field of orthopaedics continually seeks to improve our ability to help patients return to optimal function as quickly and efficiently as possible. New surgical techniques aimed at better outcomes, faster recovery, and smaller (and hopefully less painful) scars are regularly being developed and evaluated.
After nearly 2 decades, the orthopaedic community has made a good start on assuming our responsibility in the diagnosis of osteoporosis after a patient’s initial low-energy fracture. We are seeing a positive impact from programs such as the American Orthopaedic Association’s “Own the Bone” initiative as well

