JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
Month: September 2021
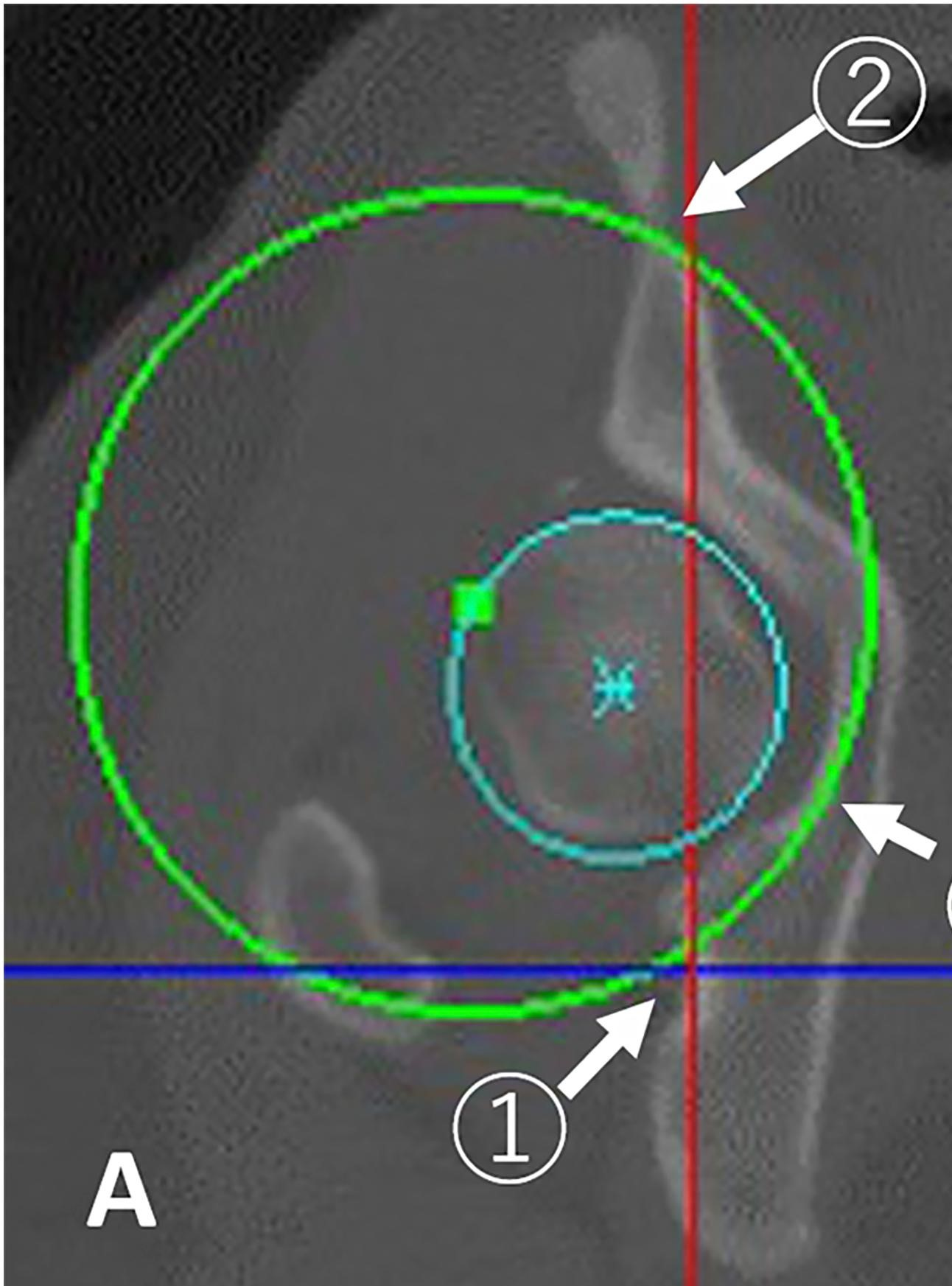
As surgeons, we are always looking to improve, or at least we should be. How can we obtain better outcomes? How can procedures be more time efficient? Can

This guest post comes from Jennifer Beck, MD. As a female, mid-career orthopaedic surgeon, I believe I bring a unique perspective to reporting on the changes that I have witnessed over the past 15

JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
JBJS is pleased once again to highlight our Elite Reviewers. The Elite Reviewers Program recognizes our best reviewers for their outstanding efforts. All JBJS reviewers
This guest post comes from David Vizurraga, MD in response to a recent JBJS Orthopaedic Forum article. Additional perspective on this topic is provided by JBJS Editor-in-Chief Dr.

JBJS is pleased to note that this year marks the 10th anniversary of JBJS Case Connector. Over the past decade, Case Connector has seen rapid growth toward its goal of

…to apply for the JBJS Robert Bucholz Journal Club Support Program for the 2021-2022 academic year. Applications are due by September 30, 2021. Please click
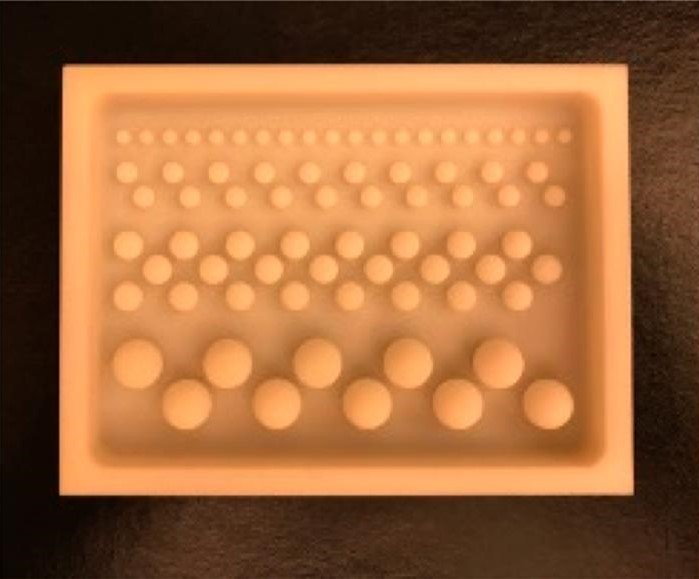
The incorporation of antibiotics within polymethylmethacrylate (PMMA) has been widely used over recent decades for managing infection following skeletal trauma. Early research helped to
This guest post comes from David Kovacevic, MD, FAAOS, who provides a summary overview of recent episodes of the OrthoJOE podcast. The July 2021 OrthoJOE podcasts from JBJS and OrthoEvidence, featuring Mohit Bhandari, MD and Marc Swiontkowski,

