Percutaneous pinning of displaced supracondylar humeral fractures (SCHFs) in children has been the treatment of choice for decades. The debate regarding all-lateral pinning versus cross-pinning with both lateral and medial pins has been ongoing for nearly as long. The rationale for all-lateral pinning is driven primarily by concern over injury to the ulnar nerve from medial pin insertion. The rate of such injury has been reported to be in the range of 1% to 3% and is easy to understand given the difficulty of palpating the medial epicondyle in an acutely injured and swollen limb in a child.
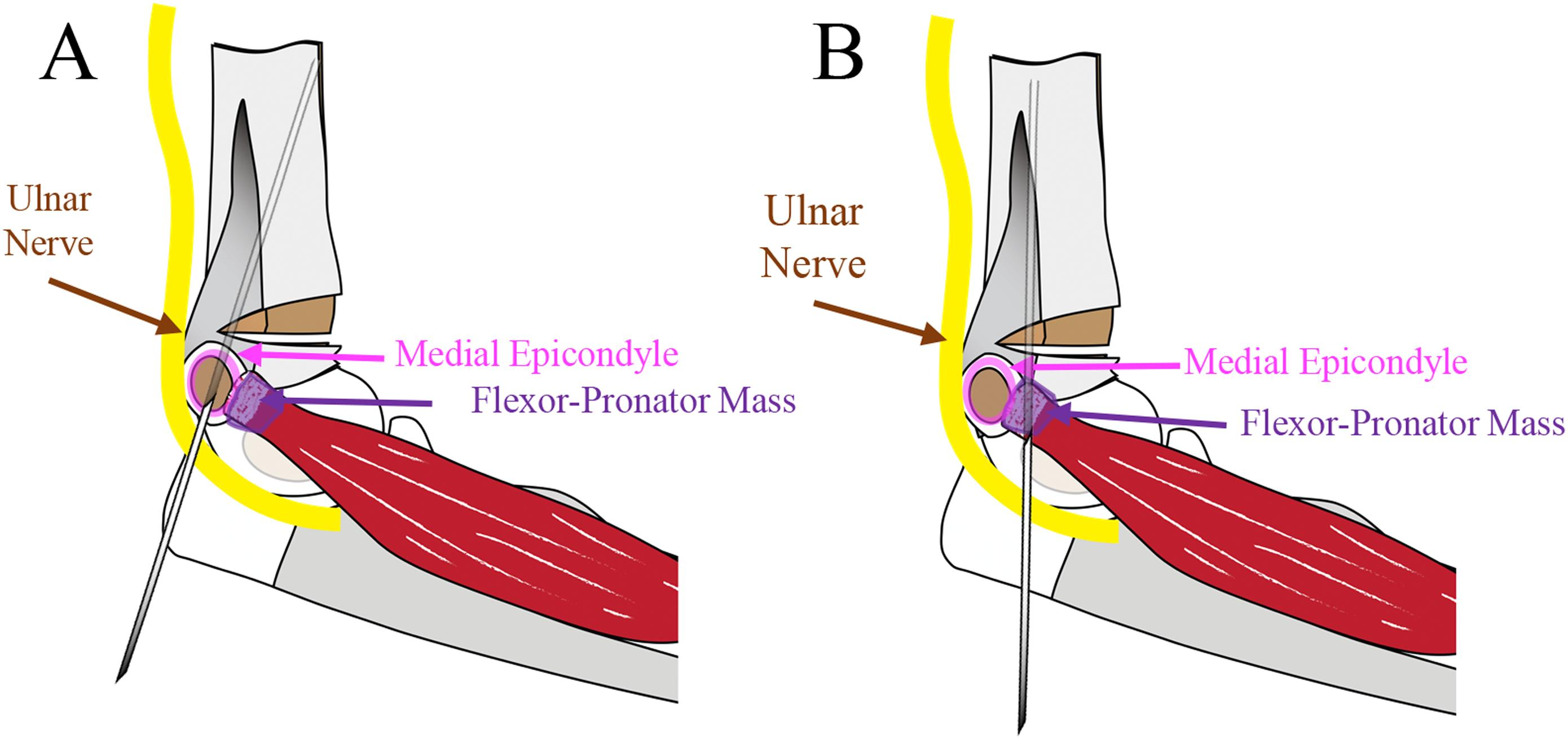
In the January 5, 2022 issue of JBJS, Rees and colleagues from Vanderbilt University Medical Center in Tennessee relate their experience with cross-pinning via the mini-open technique, involving a 1-cm incision and direct exposure of the epicondyle to enhance the safety of medial pin placement.
Among the 698 patients included in this retrospective analysis, iatrogenic ulnar nerve injury was documented for 3 patients, or 0.43% of the cases, a rate notably lower than reported estimates. One of the 3 patients sustained a direct violation of the ulnar nerve while undergoing revision pin placement, was immediately symptomatic, and had mild symptoms at the last follow-up visit (21 weeks). In the other 2 patients, the nerve symptoms were not diagnosed until the postoperative follow-up visits, and these patients had complete resolution of nerve symptoms by a mean follow-up of 15 weeks.
The authors point out that the need for medial pinning is assessed intraoperatively after the placement of 2 lateral pins and using the internal rotation stress test to evaluate the stability of the medial column. Their finding that the described technique for medial pinning may be safer than previously thought is indeed of interest to the orthopaedic community. Especially when the elbow is markedly swollen, this mini-open approach may enhance protection of the ulnar nerve so that the biomechanical benefits of cross-pinning in the treatment of unstable SCHFs can be more safely realized.
Read the full report here.
Marc Swiontkowski, MD
JBJS Editor-in-Chief