A new JBJS report compares arthroscopic versus open ankle arthrodesis. The authors analyzed long-term patient-reported outcomes, major complications, and reoperations. JBJS Editor-in-Chief Dr. Marc Swiontkowski shares his perspective on this investigation of ankle fusion procedures.
It was nearly 2 decades ago that arthroscopic techniques for ankle arthrodesis began to move into the mainstream armamentarium of specialist foot and ankle surgeons. Early published results were promising, but uptake was initially slow.
With the maturation of arthroscopic teaching tools, and increasing exposure within orthopaedic educational training programs, we’ve seen increasing utilization of the arthroscopic approach. Since implant insertion is basically the same with both open and arthroscopic techniques, advantages of the arthroscopic approach include limited incisions with concomitant limited soft-tissue stripping.
Arthroscopic Versus Open Ankle Arthrodesis
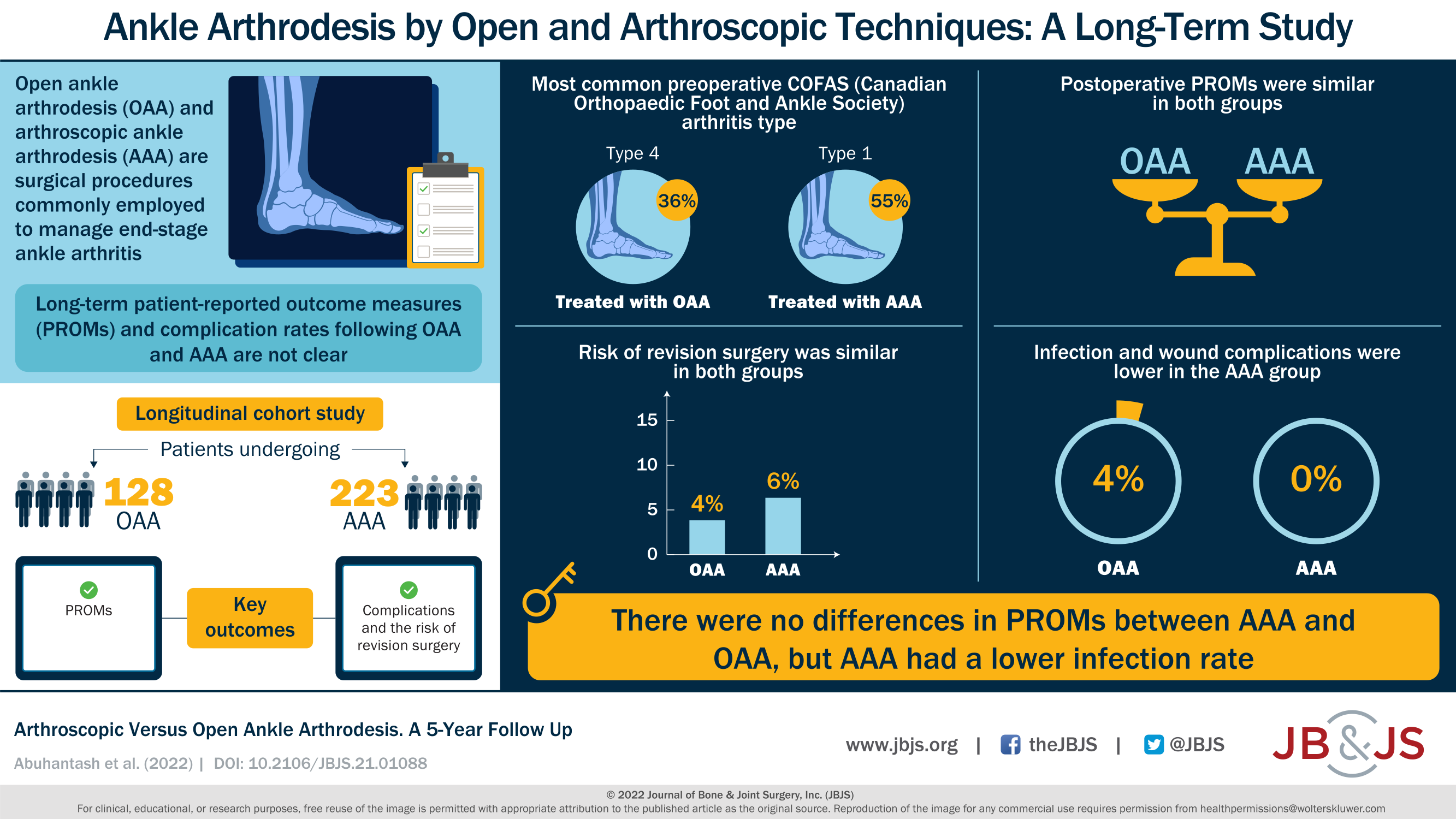
In the July 6, 2022 issue of JBJS, Abuhantash et al. report the results of an analysis of their ankle arthrodesis registry data. Patients underwent either arthroscopic arthrodesis (n = 223) or open arthrodesis (n = 128) for end-stage ankle arthritis. All procedures were performed in a single tertiary-care hospital in British Columbia, Canada. Surgeons had similar levels of experience with both procedures.
After adjusting for baseline characteristics, they found significant improvements in outcome scores in both groups at 6 months after fusion. Patient-reported outcomes did not differ between the groups from 6 months to 5 years.
The rate of revision for malunion or nonunion was 6% in the arthroscopic group compared with 4% in the open surgical group. While not a significant difference, it is possible that the higher failure rate in the arthroscopic group may be related to less optimum visualization during the removal of cartilage on the surfaces of the talus and distal tibia and fibula.
The complication rates of the 2 approaches favor the arthroscopic approach: no deep infections or wound complications occurred in the arthroscopic group, while 5 patients in the open group had such complications.
This study, although not Level I evidence, supports the continued trend in our field toward limited surgical dissection wherever it is feasible based on patient factors as well as surgeon arthroscopic skill and experience.
The full study by Abuhantash et al. can be accessed at JBJS.org.
Access the downloadable infographic of this study.
Marc Swiontkowski, MD
JBJS Editor-in-Chief
For related reading, see the JBJS Clinical Summary on ankle arthritis. And from OrthoBuzz: “What’s New in Foot and Ankle Surgery 2022.”




I must admit being astonished about the focus of the attention to the technique for ankle fusion. Instead of concentrating our thoughts on the way how to fuse the joint we should think about the essentials: remaining fuction after the surgery. One of the them is the length of the fibula and the routing of the fibular tendons. Another one is the approach which does minimal harm from postero-lateral and last but not least, the orientation of the foot in relation to the knee axis which allows optimal function of the remaining talo-calcaneo-navicular motion.