There are some orthopaedic conditions for which a delay in treatment of even a few hours can lead to poor outcomes. Septic arthritis (SA) is one of those conditions. Bacteria can be extremely destructive to cartilage within joints.
Culture results from joint aspiration represent the gold standard in diagnosing SA. However, given the time-critical nature of SA, surgeons have used a synovial fluid white blood-cell count (SF-WBC) of >50,000 cells/mm3 or >90% polymorphonuclear leukocytes (%PMN) as the initial diagnostic criterion.
In the current issue of JBJS, Varady et al. report on a novel biomarker for assessing SA in patients with native joint infections: the neutrophil-to-lymphocyte ratio (NLR). In non-orthopaedic conditions, the NLR has been shown to be a helpful biomarker suggestive of systemic inflammation, which leads to an increase in neutrophils and a decrease in lymphocytes associated with the stress response. Elevated serum NLR has also been identified as a prognostic marker for select orthopaedic conditions. However, its utility in the diagnosis and prognosis of SA is not fully known.
Study Highlights
The authors retrospectively reviewed 598 adult patients with suspected bacterial SA of the native shoulder, hip, or knee (2000 to 2018). The patients underwent joint aspiration with synovial fluid analysis.
Laboratory markers collected included the SF-WBC, SF-absolute neutrophil count, and SF-absolute lymphocyte count. The NLR was determined by dividing the absolute neutrophil count by the absolute lymphocyte count. The %PMN was determined by dividing the absolute neutrophil count by the WBC.
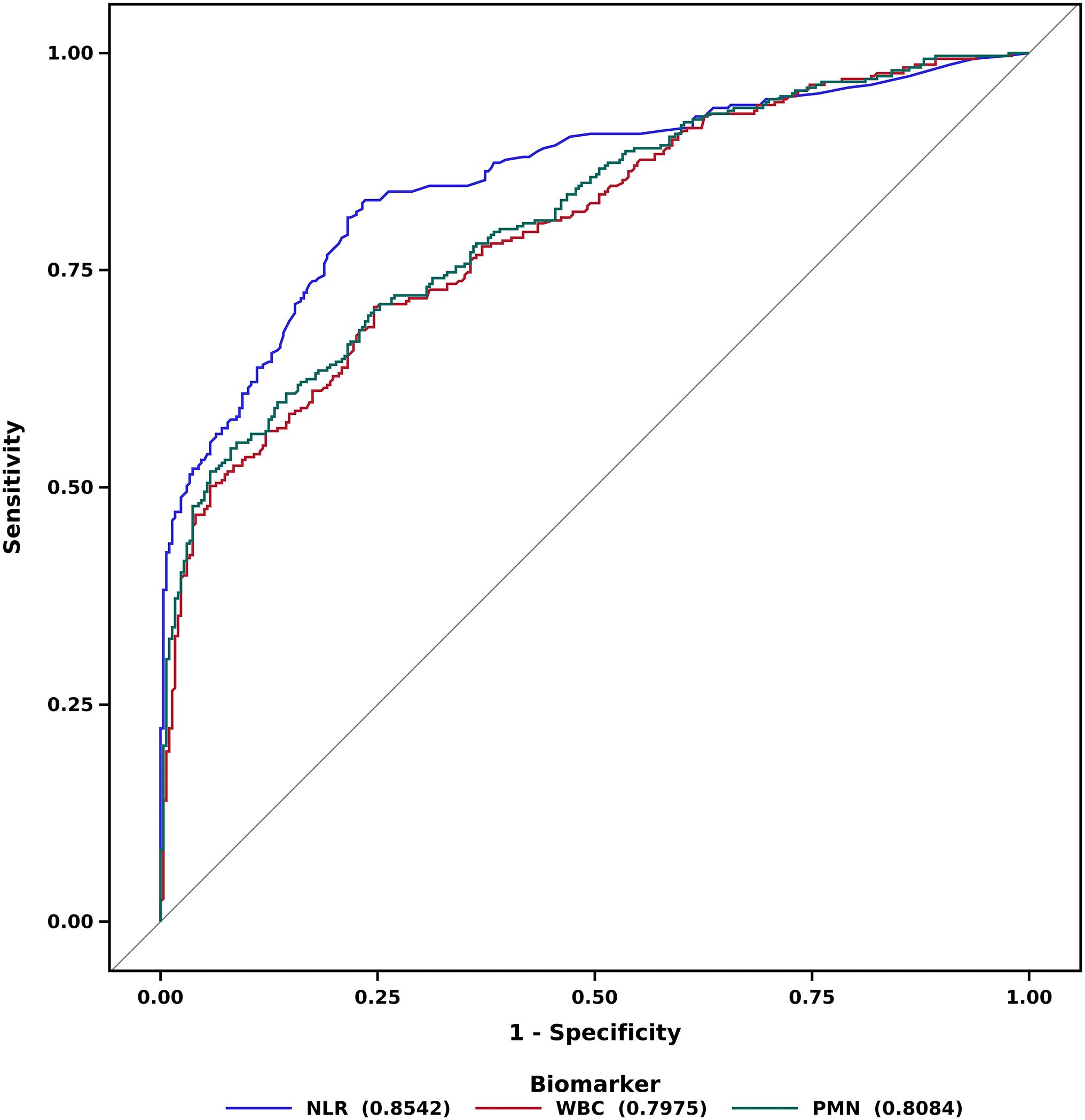
The authors computed receiver operating characteristic (ROC) curves. Diagnostic accuracy was determined from the associated area under the ROC curve (AUC). The results were compared with traditional criteria for diagnosing SA.
A secondary analysis of 235 patients with confirmed SA was performed to assess the prognostic ability of serum NLR.
Findings Compared with Traditional Markers
The investigators found that the optimal threshold of the SF-NLR was 25, as determined by the Youden index (highest value of sensitivity plus specificity). The SF-NLR was significantly more accurate for diagnosing SA than the SF-WBC (p = 0.002) and SF-%PMN (p = 0.01). Of the 235 people identified with SA who had a full serum workup, the serum NLR was significantly more accurate for a poor prognosis than was C-reactive protein level (p = 0.01) and erythrocyte sedimentation rate (p < 0.001).
In a multivariate analysis controlling for patient demographics, comorbidities, and social factors, elevated serum NLR was independently associated with 90-day treatment failure and mortality.
Compared to the typical criterion of an SF-WBC of >50,000 cell/mm3 (56% sensitivity and 80% specificity) or SF-%PMN of >90% (65% sensitivity and 78% specificity), the NLR exhibited both a higher sensitivity (78%) and specificity (81%) at the optimal threshold of 25. As the authors explain, SF-NLR of >25 would have accurately diagnosed 22% of SA cases that would have been missed using SF-WBC of >50,000 cell/mm3, while misdiagnosing 1% fewer cases of non-SA. In addition, SF-NLR would have identified 12% of the cases missed by SF-%PMN of >90%, while misdiagnosing 3% fewer cases.
The findings from this retrospective study need to be validated, preferably in a multicenter prospective study. Nonetheless, the study points to a potentially more accurate and rapid diagnostic test to aid in identifying SA.
According to the authors, “Given that the NLR is simply a recalculation of data already routinely collected, it can be used immediately—without any added costs—to aid clinicians in improving the diagnosis and prognostication of SA.”
Learn more about the study from co-author Nathan H. Varady, MD, MBA in this Author Insights video.
Matthew R. Schmitz, MD
JBJS Deputy Editor for Social Media




El gran reto del diagnostico temprano de la artritis septica, en forma usual se emplea la VSG velocidad de sedimentacion y la BH completa, actualmente se puede anexar el USG