Trochanteric fractures often occur in older patients, including those with osteoporosis, and are associated with high rates of mortality and morbidity.
Investigators previously conducted a randomized controlled trial to evaluate outcomes of fixation with the Proximal Femoral Nail Antirotation, or PFNA, using cement augmentation (TRAUMACEM V+ Injectable Bone Cement) vs. no augmentation in patients with closed, unstable trochanteric fractures1. They found a trend toward a reduced risk of implant-related revision when cement augmentation was used.
In the current issue of JBJS, Joeris et al. examine whether this reduced risk may result in long-term cost savings.
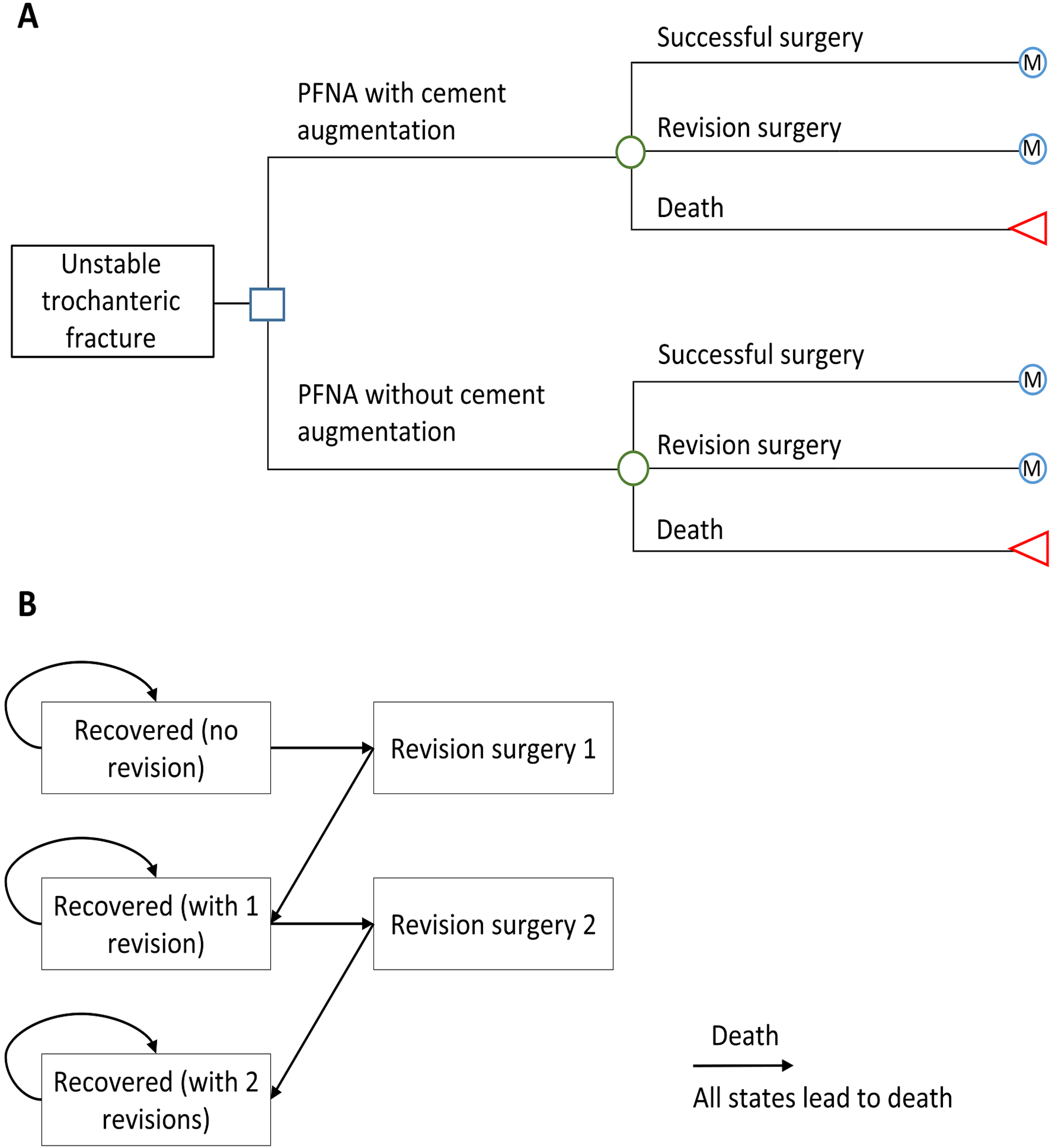
- Cost-effectiveness from the German health-care payer’s perspective was assessed. The model included 2 stages. A short-term decision tree model simulated clinical events and their associated costs and utilities in the first year following fracture fixation. A Markov state-transition model extrapolated clinical events, costs, and utilities over the patients’ lifetime. The previous RCT, current literature, and administrative claims data served as sources of the model parameters.
- Incremental costs (in Euros), incremental quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratios (ICERs) were the outcome measures.
The researchers found that fixation with cement augmentation (vs. no augmentation) was the dominant strategy in the analysis, mainly because of cost savings.
As reported by the authors:
“The base-case analysis showed that fixation with cement augmentation was the dominant strategy as it was associated with cost savings (€50.3/patient) and QALY gains (0.01 QALY/patient). Major influential parameters for the ICER were the utility of revision, rates of revision surgery within the first year after fixation surgery, and the costs of augmentation and revision surgery. Probabilistic sensitivity analyses demonstrated that estimates of cost savings were more robust than those of increased QALYs (66.4% versus 52.7% of the simulations). For a range of willingness-to-pay thresholds from €0 to €50,000, the probability of fixation with cement augmentation being cost-effective versus no augmentation remained above 50%.”
The authors state that further studies are needed to assess the generalizability of their findings to other cement augmentation techniques and to assess whether cement augmentation is more cost-effective among patients with a greater risk of revision surgery than in the population evaluated. And they point to the need for future analyses when data on the long-term costs and effectiveness of cement augmentation are available.
Their results, note the authors, “could provide policy-makers with useful information about the cost-effectiveness of cement augmentation from the health-care payer’s perspective when deciding on hospital reimbursement schemes.”
Read the full report by Joeris et al., now freely available at JBJS.org.
References:
- Kammerlander C, Hem ES, Klopfer T, Gebhard F, Sermon A, Dietrich M, Bach O, Weil Y, Babst R, Blauth M. Cement augmentation of the Proximal Femoral Nail Antirotation (PFNA) – A multicentre randomized controlled trial. Injury. 2018 Aug;49(8):1436-44.