Dr. Marc Swiontkowski, JBJS Editor-in-Chief, offers his thoughts on a new randomized controlled trial comparing primary closure and secondary wound healing of pin sites after temporary external fixation.
External fixation remains a frontline treatment option for severe open fractures in the upper and lower extremities. Its use in lower-grade open fractures has waned as relevant clinical trials have identified better treatment outcomes with intramedullary nailing in the lower extremity and plate fixation in the upper extremity. Its use for the temporary stabilization of closed and open periarticular fractures, particularly around the knee and ankle, has expanded in the last decade and a half. Stabilization of the limb while maintaining skeletal length, to allow swelling to subside while definitive treatment planning occurs, has been a major advance.
In the February 1, 2023 issue of JBJS, Tillmann et al. explore a clinically relevant question regarding the management of pin-site incisions when temporary frames are removed: “Is primary closure of these incisions at the time of fixator removal safe?”
Concerns regarding infection are real. However, most of these infections occur in cases in which the external fixator has been in place for 1 to 3 months. The temporary frames are generally removed in 7 to 10 days or less.
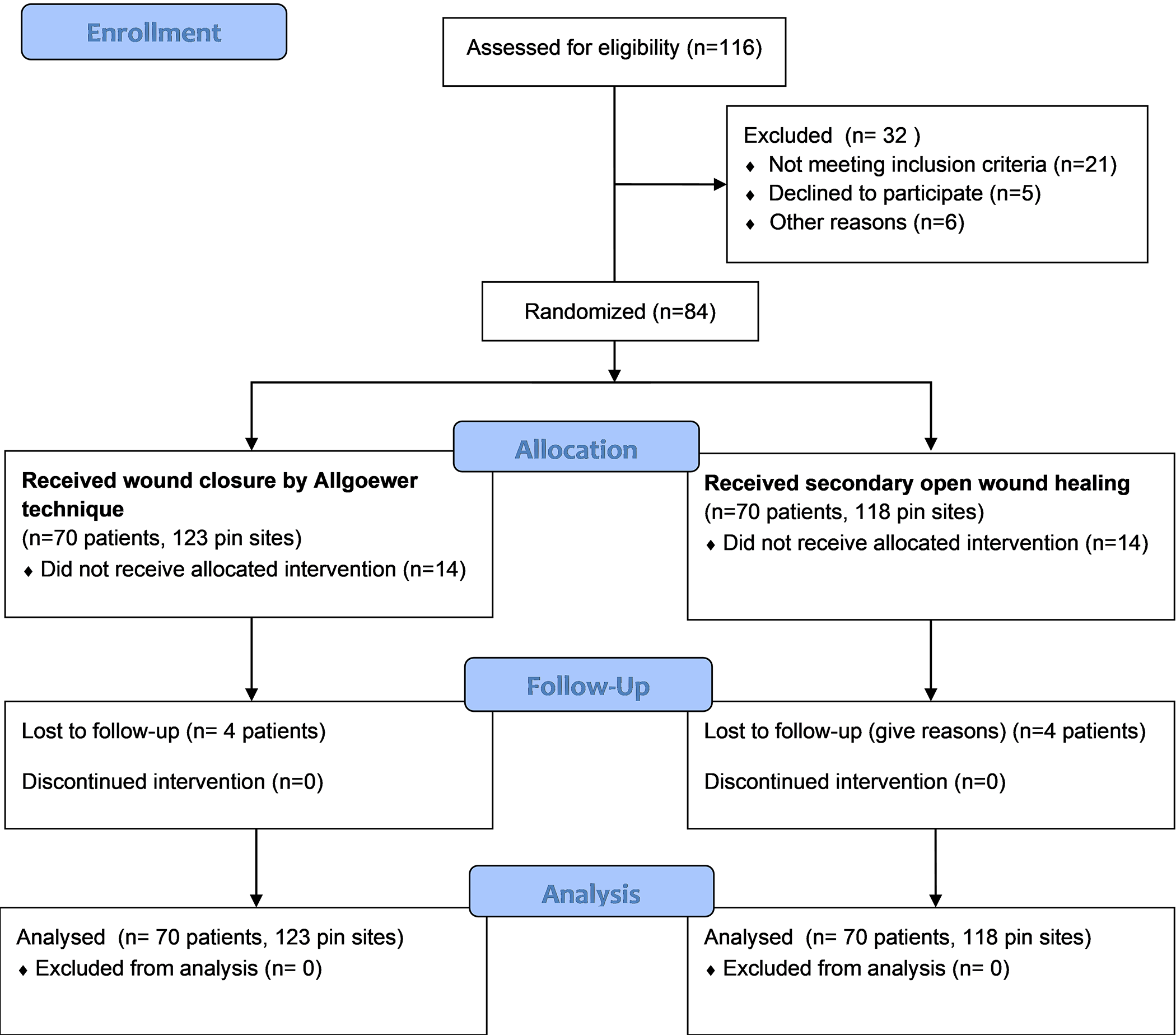
Tillmann and colleagues evaluated primary wound closure using a suture vs. secondary wound healing of pin sites following temporary external fixator removal.
Study Highlights
- This was a Level-I noninferiority randomized controlled trial performed at a single center in Lucerne, Switzerland. Patients were treated with a temporary external fixator on an upper or lower extremity. The median duration of external fixation was 6 days.
- A total of 70 patients (241 pin sites) were included in the analysis: 123 pin sites were treated with primary closure, and 118 were treated with secondary wound healing. The median patient age was 55 years, and 44% of the patients were male.
Findings
- No pin-site infections occurred in either group. One case of fracture-related infection, unrelated to a pin site, was reported.
- Wound healing was significantly faster in the group treated with primary closure (median of 2 vs. 6 weeks; p = 0.013). At 2-week follow-up, 82% of the sites had healed in the primary closure group vs. 61% in the secondary wound healing group (p = 0.001).
- The 2 groups did not differ in terms of the Vancouver Scar Scale (VSS), patient satisfaction, or VAS for pain.
The authors note that the overall infection rate they observed is lower than typically reported and that this could be explained in part by their definition of infection (requiring intervention). In addition, they note the strict protocol for pin-site treatment among limitations of the study in terms of generalizability.
Nevertheless, their findings suggest that primary closure of pin sites for frames that are used for a limited duration should be considered as the standard of care for appropriate patients.
Access the full study at JBJS.org.
JBJS Editor-in-Chief
Recent OrthoBuzz posts:
Announcing JBJS Media: Gold-Standard Video Content All in One Place at JBJS.org
Resident Roundup: Persistence in Ortho
Periacetabular Osteotomy in the Setting of Borderline Hip Dysplasia