In this post, JBJS Editor-in-Chief Dr. Marc Swiontkowski discusses a new study evaluating patients’ treatment preferences and expectations in the management of radial nerve injuries.
Radial nerve palsy presents in 10% to 20% of cases of humeral shaft fracture, particularly in distal one-third shaft fractures. Nearly as common is the presence of a postoperative palsy associated with open surgical stabilization. In both clinical scenarios, full or partial recovery of sensory and motor function occurs in nearly 90% of patients, as the nerve injury is a traction, or neuropraxia, injury which recovers over 2 to 6 months. When it is clear that nerve recovery is not forthcoming, the choices are splinting with “expectant” treatment, tendon transfer, or nerve transfer. Little comparative outcome data are available for these 3 options.
In the era of level-of-evidence-framed data, subjective patient interview data have become increasingly important to help inform our interpretation of clinical trial data. In the current issue of JBJS, Lieberdorfer et al. present the results of their interviews with 15 patients with radial nerve injuries (5 expectant management, 5 tendon transfer only, and 5 nerve transfer, with or without concomitant tendon transfer).
Thirteen patients had an isolated humeral fracture related to their nerve injury (10 traumatic and 3 iatrogenic nerve injuries). The 2 remaining patients had iatrogenic injuries from reverse shoulder arthroplasty and rotator cuff repair.
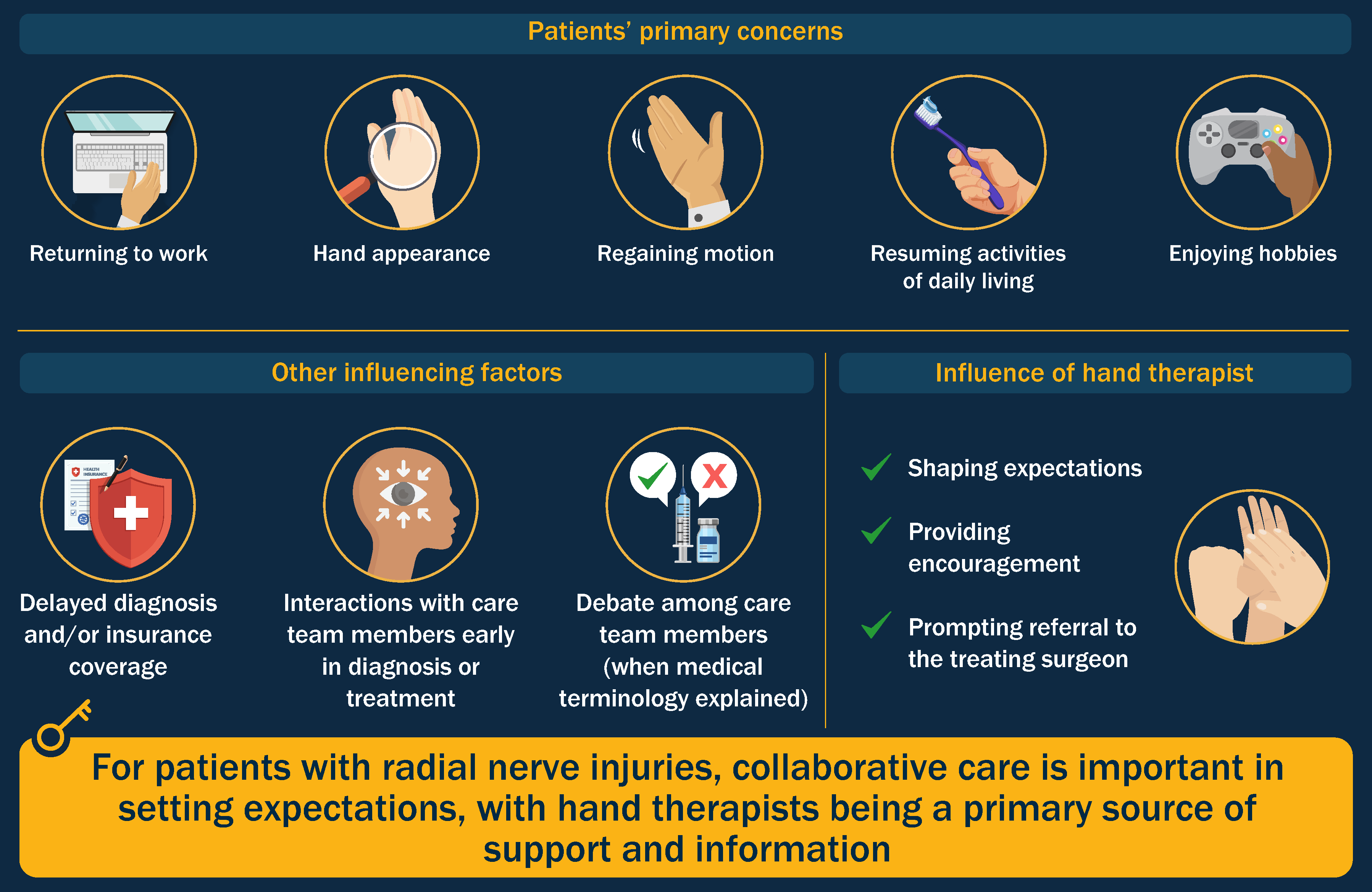
The authors used a semi-structured interview design to collect and record patients’ perceptions and experiences related to injury diagnosis, treatment decision-making, and expectations. It is no surprise that early interactions with members of the care team strongly influenced perceptions of the treatment experience, and that of the team members, hand therapists were the most influential in shaping expectations.
Five groups of themes emerged from the interviews: initial concerns prior to treatment, understanding of injury, goals for treatment, expectations of treatment and recovery, and interactions with health-care providers. Regarding the latter, some participants noted that receiving contradictory information early on was stressful and that there were times when information was relayed when they were not ready to receive it (e.g., late at night). Three patients “crossed over” from nerve transfer to tendon transfer, reporting diagnosis or insurance coverage delay. Helpful communication strategies included quantifying progress with concrete milestones, explaining medical terminology, and open discussion among care team members, which reinforced patient trust.
Overall, the authors note that their findings highlight the importance of initial, collaborative care in setting expectations.
We at JBJS continue to emphasize research methodology that limits bias as a metric when adopting research findings into clinical decision-making. It is becoming clearer over time that “softer” data relating the patient experience, such as in this study, should also be part of the research fabric for shared treatment decision-making. Both approaches help us as physicians and surgeons when consulting with patients as they seek to understand what is the best treatment approach for their disease or injury.
The study by Lieberdorfer et al., along with a downloadable infographic, can be found at JBJS.org.
JBJS Editor-in-Chief