This post comes from Dr. Matt Schmitz, JBJS Deputy Editor for Social Media. He reflects on a new study evaluating the impact of an allograft-reduction intervention for anterior cruciate ligament (ACL) reconstruction that was implemented across one health-care system.
All of us involved in medical research understand the importance of scientific questions and interpreting results that come out of the academic literature. It is one thing to have a study published in a peer-reviewed medical journal, but it is another thing altogether for that study to become “practice-changing” and its findings incorporated into everyday medical care for our patients.
In the April 19, 2023 issue of JBJS, Maletis et al. present the results of a study in which they evaluated the change in practice habits of surgeons and clinical outcomes of patients following an allograft-reduction intervention for anterior cruciate ligament (ACL) reconstruction. The intervention was implemented throughout the Kaiser Permanente system on the basis of study findings and with tracking and feedback via a clinical registry.
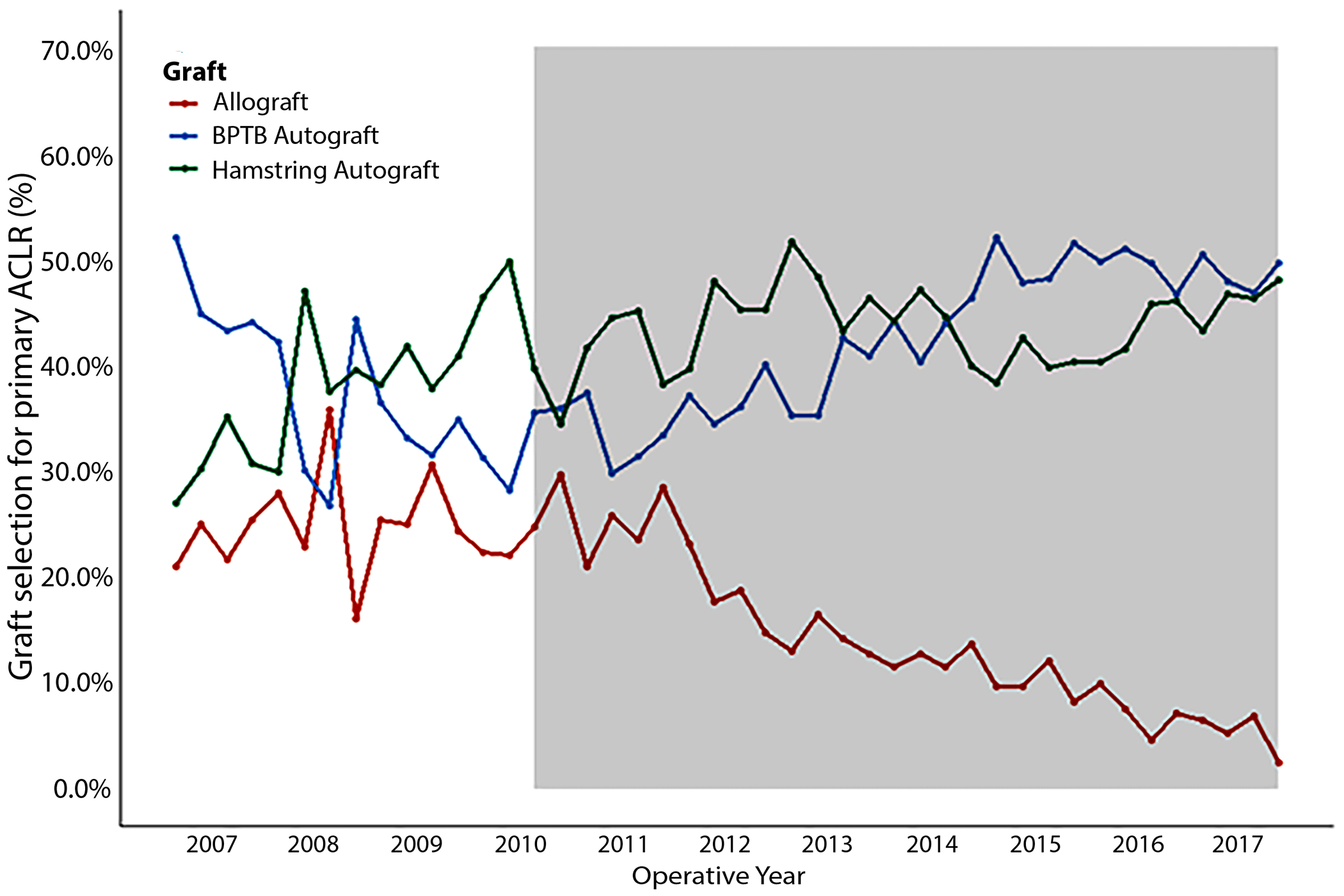
In the last decade, multiple studies showed higher failure rates in ACL reconstruction of young athletes when utilizing allograft compared with autograft. Kaiser implemented an intervention to decrease the use of allografts in favor of autografts, specifically in primary ACL reconstructions in higher-risk patients ≤21 years of age. Communication channels included internal conferences, presentations, newsletters, and utilization reports. In addition to evaluating the impact of the intervention on reducing allograft utilization, the investigators looked at whether revision rates changed, employing an interrupted time series study to measure longitudinal effects of population-level interventions.
Study Highlights
The Kaiser ACL Reconstruction Registry was utilized with surgeon input and supplemented with data from the health record. Voluntary participation in the registry was >90% during the period of study. The final cohort for the analysis included 11,808 patients ≤21 years of age who underwent ACL reconstructions between January 1, 2007 and December 31, 2017 and had a minimum of 2 years of follow-up. The first report from the registry describing the higher risks with allograft tissue was disseminated throughout the health-care system in the fourth quarter of 2010, so the pre-intervention period entailed 15 quarters (January 1, 2007 to September 30, 2010) and the post-intervention period, 29 quarters (October 1, 2010 to December 31, 2017).
- Allograft utilization increased pre-intervention from 21.0% in 2007 Q1 to 24.8% in 2010 Q3. Utilization then decreased post-intervention from 29.7% in 2010 Q4 to 2.4% in 2017 Q4.
- The quarterly 2-year revision rate increased pre-intervention from 3.0 to 7.4 revisions per 100 ACL reconstructions. Using the pre-intervention trend, the authors predicted that the revision rate for 2017 Q4 would have been 14.7 revisions per 100 ACL reconstructions but found that the intervention decreased the actual revision rate to 4.1 per 100 ACL reconstructions for that quarter.
- Utilizing regression analysis, they found that the revision rate over time increased pre-intervention (relative risk [RR], 1.03; 95% confidence interval [CI], 1.00 to 1.06 per quarter), while it decreased post-intervention (RR, 0.96; 95% CI, 0.92 to 0.99 per quarter). In simple terms, they observed a 3% increase in the 2-year revision rate relative to the prior quarter pre-intervention and a 4% decrease in the rate relative to the prior quarter post-intervention.
Impact on Outcomes
This study shows that we can utilize clinical research to impact patient outcomes on a large scale with proper interventions. The surgeons at Kaiser were able to decrease the use of allograft tissue in higher-risk ACL reconstructions while also decreasing the 2-year revision rate. What we read in the orthopaedic literature can be used to help patient outcomes when we correctly interpret evidence-based findings and then implement related changes on a practice or system-wide basis. To me, this speaks to the main reason we perform research, and to the mission of JBJS: to improve clinical outcomes for our patients.
A downloadable infographic is available with this study: An Interrupted Time Series Analysis Measuring the Impact of Research and Education on Clinical Practice: Decreasing Allograft Use in Young Patients Using a Registry to Track Outcomes
JBJS Deputy Editor for Social Media