Editor-in-Chief Dr. Marc Swiontkowski discusses a new study from The Netherlands that presents a fully automatic method for assessing lower-limb alignment from computed tomography (CT) scans.
Lower-limb malalignment may be associated with substantial symptoms and functional disability. Often, malalignment in the hip, knee, or ankle is not amenable to treatment with therapeutic exercise or bracing. The most important step is conducting a physical exam with the patient ambulating and in the seated, prone, and supine positions. If malalignment is detected, the next step is imaging. This is generally in the form of full-length radiographs and CT scans. The use of EOS imaging has been a major advancement as the importance of 2D and 3D assessment has been clarified.
The measurement of alignment parameters is critical in surgical treatment planning. Reproducibility and precision are key.
In the May 3, 2023 issue of JBJS, Kuiper et al. describe a new computational system for the assessment of lower-limb alignment from CT scans.
Automatic Assessment of Lower-Limb Alignment from Computed Tomography
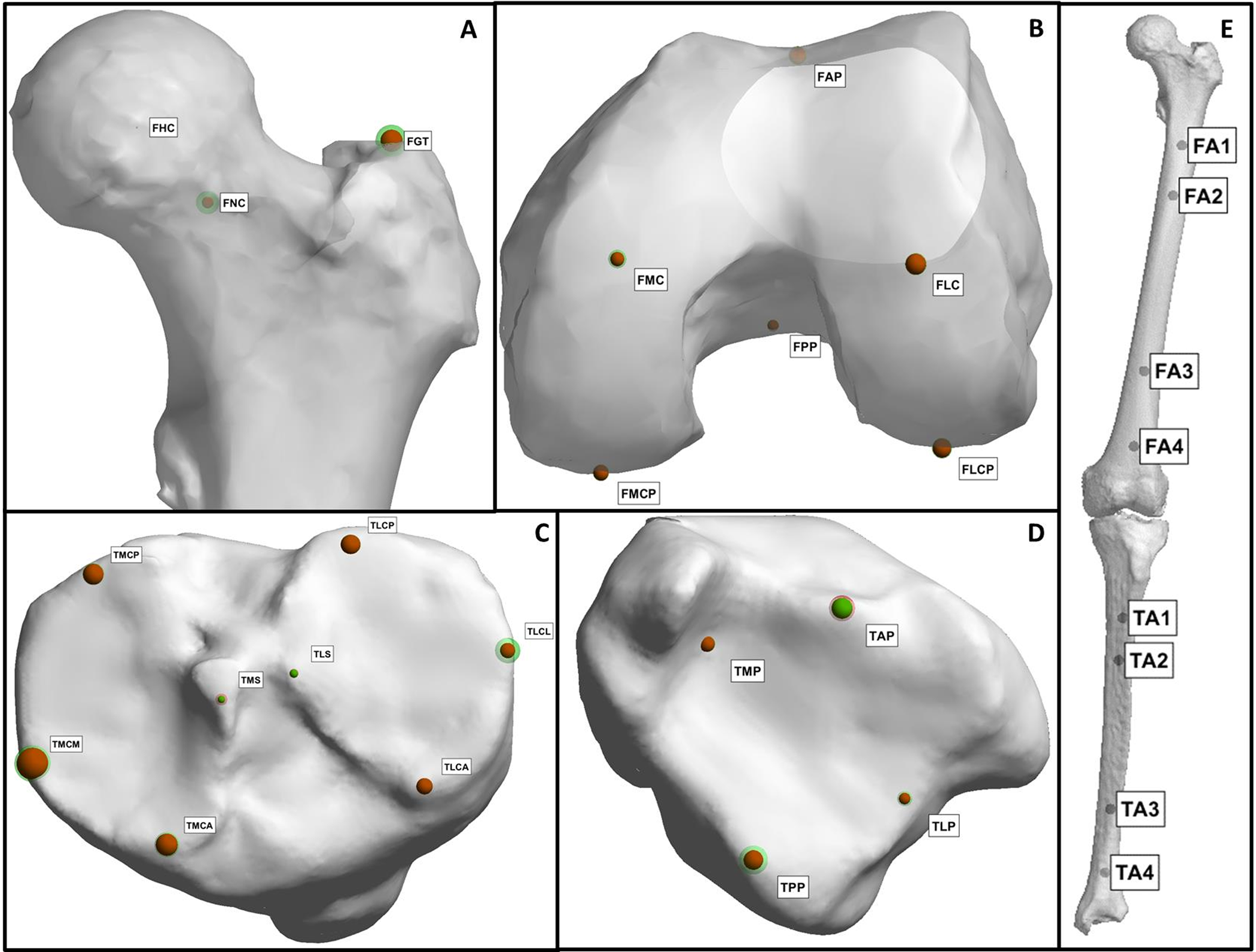
Bilateral, non-weight-bearing, lower-extremity CT scans of 50 subjects in the supine position were obtained retrospectively; the subjects had no previous indication of lower-limb malalignment. The CT scans were both manually and automatically segmented. Manual and automatic methods were used to position landmarks. The landmarks were then used to calculate 25 angles describing lower-limb alignment. Details of the manual and automatic workflows are presented by the authors along with the definitions of all landmarks used and angles calculated.
The investigators conducted careful reproducibility assessments of the manual measurements and comparisons between manual and computational system assessments (including semi- and fully automatic workflows).
Of note, the manual method averaged 1 hour of time (approximately 40 minutes per leg for segmentation and 20 minutes per leg for landmark positioning). In contrast, the fully automatic workflow required approximately 12 minutes of computation time (10 minutes for segmentation and 2 minutes for landmark positioning).
When assessing repeat measurements using the manual method, the authors found that the mean absolute difference was 2.01 ± 1.64 mm for the landmark positions and 1.05° ± 1.48° for the landmark angles. Comparing the manual and fully automatic methods, the mean difference was 2.17 ± 1.37 mm for the landmark positions and 1.10° ± 1.16° for the landmark angles. The computational system was demonstrated to be as accurate as the human observers, while requiring substantially less time to obtain calculations.
Good to excellent reliability between the manual and fully automatic assessments was found for 23 of 25 of the angles, which was similar to the intraobserver reliability of the manual method. For 18 of 25 angles calculated automatically, the mean for the 50 subjects was within the expected normal range.
I believe that the impact of the authors’ findings is underemphasized. It would be rare for a clinician to spend 60 minutes on measurements in surgical planning. Thus, measurement error may be greater than what is presented in this study. To have this computational system available for clinical application represents a major advance. It is my hope that widespread dissemination of the program will follow rapidly.
Read the full study: Automatic Assessment of Lower-Limb Alignment from Computed Tomography
JBJS Editor-in-Chief
Recent Editor’s Choice posts on OrthoBuzz
Clinical Research Changing Practice and Outcomes: A Study in ACL Reconstruction
Management of Radial Nerve Injuries with Humeral Shaft Fractures: What Do Patients Say?
Catastrophic Health Expenditure: A Secondary Trauma for Many Patients




very nice article very informative