JBJS Deputy Editor for Social Media Dr. Matt Schmitz reflects on a new study evaluating postoperative complications and mortality in patients who had a recent COVID-19 diagnosis prior to elective total joint arthroplasty (TJA).
Now more than 3 years since the start of the pandemic, orthopaedic surgeons throughout the U.S. are likely tired of discussing COVID-19 and its impact on surgical practices. In 2020 and 2021, it crippled the performance of elective surgical procedures as many hospital systems diverted resources as well as feared poor outcomes for patients who had a recent COVID diagnosis.
COVID-19 hospitalizations are creeping up (again) in parts of the U.S., making a recent study by Pincavitch et al. in the current issue of JBJS quite timely:
The authors utilized the National COVID Cohort Collaborative (N3C) Data Enclave for this study. At the time of their investigation, 64 academic clinical sites from across the U.S. contributed to the N3C Data Enclave, with approximately 11.9 million patients and 4.3 million COVID-19-positive patients included in the database. The researchers sought to evaluate the risk of postoperative complications and 30-day mortality following TJA in patients with a positive COVID-19 diagnosis prior to surgery.
Specifically, they analyzed total hip arthroplasty (THA) and total knee arthroplasty (TKA) procedures between January 2018 and February 2022. They grouped patients according to COVID-19-positive or negative status, with positive diagnosis based on positive polymer chain reaction (PCR) and/or antigen test, antibody test, or clinical diagnosis prior to TJA, and negative status based on a negative test and no diagnosis of COVID-19 within 90 days before surgery. The COVID-19-positive patients were further divided on the basis of the timing of diagnosis: 0 to 14, 15 to 30, 31 to 60, and ≥61 days before surgery.
They studied baseline patient characteristics (sex, race, body mass index), type of surgical procedure (primary vs. revision), and medical comorbidities (coronary artery disease, diabetes, chronic obstructive pulmonary disease, and congestive heart failure). They also looked at postoperative complications including venous thromboembolisms, pneumonia, surgical site infections, deep surgical site infections, acute myocardial infarction (AMI), sepsis, readmissions, and 30-day mortality.
Results
Of 85,047 patients who underwent elective TJA during the study period:
- 81,531 (95.9%) were COVID-19-negative
- 3,516 (4.13%) were COVID-19-positive
In terms of medical comorbidities, more patients in the COVID-19-positive vs. negative group had diabetes (p < 0.001). Rates of chronic obstructive pulmonary disease and congestive heart failure did not differ between the 2 groups.
Univariate analysis showed significant differences in postoperative complications between the COVID-19-positive and negative groups:
- Pneumonia within 30 days occurred most often among patients who were COVID-19-positive (p = 0.027).
- The rates of AMI within 30 days (p = 0.011) and sepsis within 90 days (p = 0.009) were higher in the COVID-19 positive group.
- Readmission within 30 days occurred more often in the COVID-19-positive group (p = 0.002).
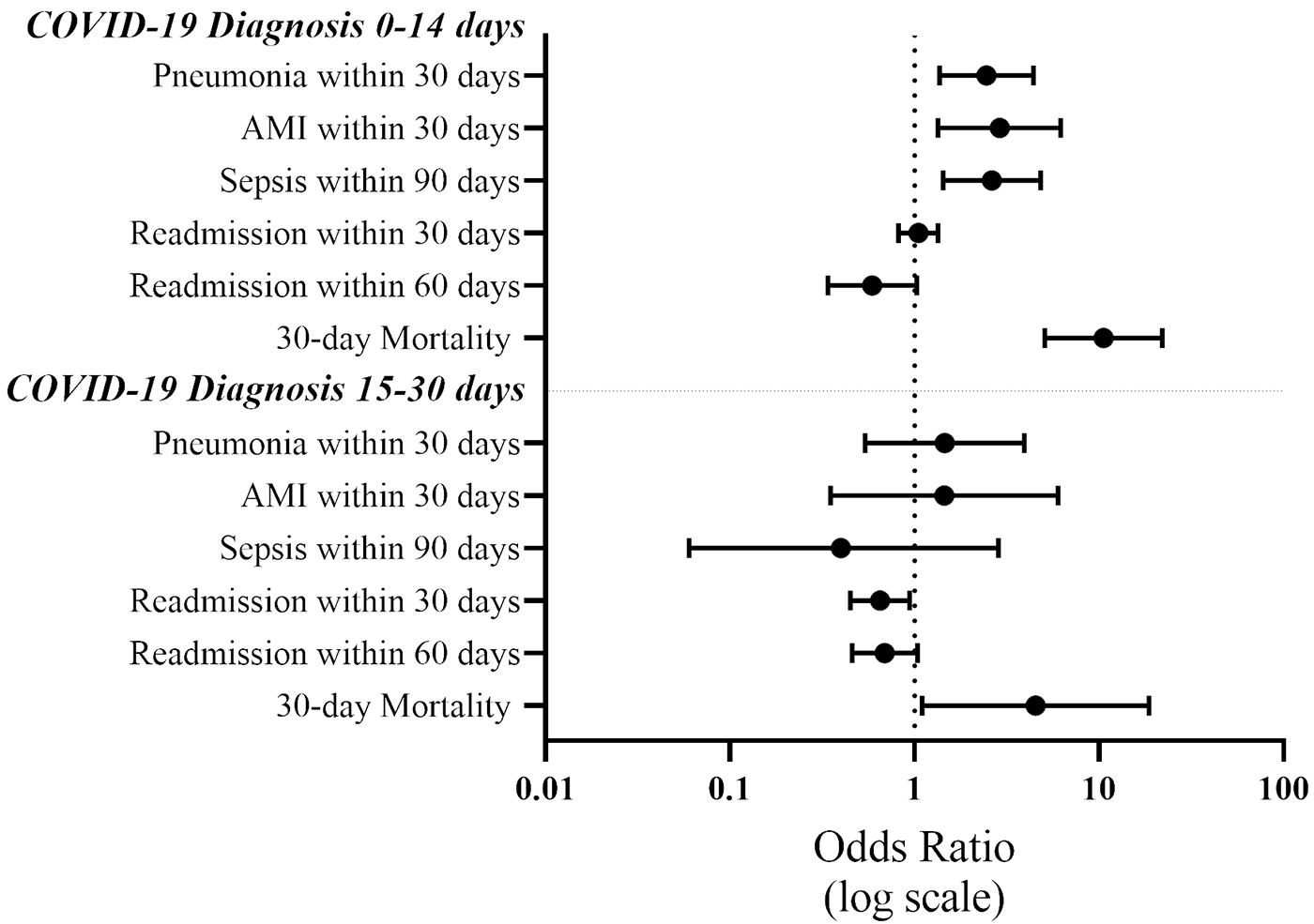
On multivariate analysis, patients with a COVID-19 diagnosis 0 to 14 days prior to TJA had:
- The highest odds of developing pneumonia within 30 days postoperatively (odds ratio [OR], 2.46; p = 0.003)
- Increased odds of an AMI within 30 days (OR, 2.90; p = 0.007)
- Increased odds of 30-day mortality (OR, 10.61; p < 0.001)
- Increased risk of sepsis within 90 days (OR, 2.63; p = 0.003).
Even with COVID-19 diagnosis 15 to 30 days prior to surgery, there was a significant increase in the odds of 30-day mortality (OR, 4.54; p = 0.036).
In summary, a recent diagnosis of COVID-19 was associated with multiple deleterious effects on outcomes for patients undergoing TJA, especially if that diagnosis was within 2 weeks prior to surgery. The authors note that their findings be interpreted with caution given that the data were collected “over a large period of time where the emergence of different variants, vaccination status, and prevalence could have impacted results.”
Nonetheless, data from this study may help inform conversations with patients undergoing elective joint arthroplasty, especially as the number of COVID-19 cases begins to rise yet again.
JBJS Deputy Editor for Social Media
Access the full report at JBJS.org: Thirty-Day Mortality and Complication Rates in Total Joint Arthroplasty After a Recent COVID-19 Diagnosis: A Retrospective Cohort in the National COVID Cohort Collaborative (N3C)
Additional perspective on this study is provided in a commentary by Dipit Sahu, MS(Ortho): Performing Total Joint Arthroplasty on Patients with a Recent COVID-19 Diagnosis Carries an Increased Risk of Postoperative Complications