In a new study in JBJS, Novais et al. note the challenge of treating patients with symptomatic hips after healed Legg-Calvé-Perthes disease (LCPD) given the complexity of the deformity. Surgical hip dislocation (SHD) is often used in treating residual deformity related to LCPD, and previous studies have demonstrated short-term improvement following SHD when performed with concomitant procedures. “However,” state the researchers, “most published studies were limited to early findings with short-term follow-up. It is therefore still unclear from the literature whether SHD and related procedures retain hip function, preserve the native hip, and avoid total hip arthroplasty (THA) in the intermediate and long term.”
Their new retrospective study evaluates mid-term outcomes of SHD with femoral-head reshaping and relative femoral-neck lengthening. The study is now available at JBJS.org:
- Sixty patients who underwent SHD for the treatment of symptomatic residual LCPD deformity were identified. Fifty-one (85%) were followed for ≥4 years postoperatively (21 male and 30 female patients).
- The mean patient age at surgery was 16.3 years.
- Surgical failure was defined as conversion to, or recommendation for, total hip arthroplasty or a WOMAC pain score of ≥10 (moderate pain or worse) at the most recent follow-up.
- Predictors of surgical failure and survival rate were also assessed.
Highlights of Findings
The investigators found that 20 (39%) of the patients met 1 of the end-point criteria for surgical failure. Hips of the remaining 31 (60%) of the patients were successfully preserved at a median follow-up of 10.2 years.
On Kaplan-Meier analysis, the estimated rate of survival free from failure was 80% (95% confidence interval [CI] = 70% to 92%) at 5 years and 66% (95% CI = 53% to 81%) at 10 years.
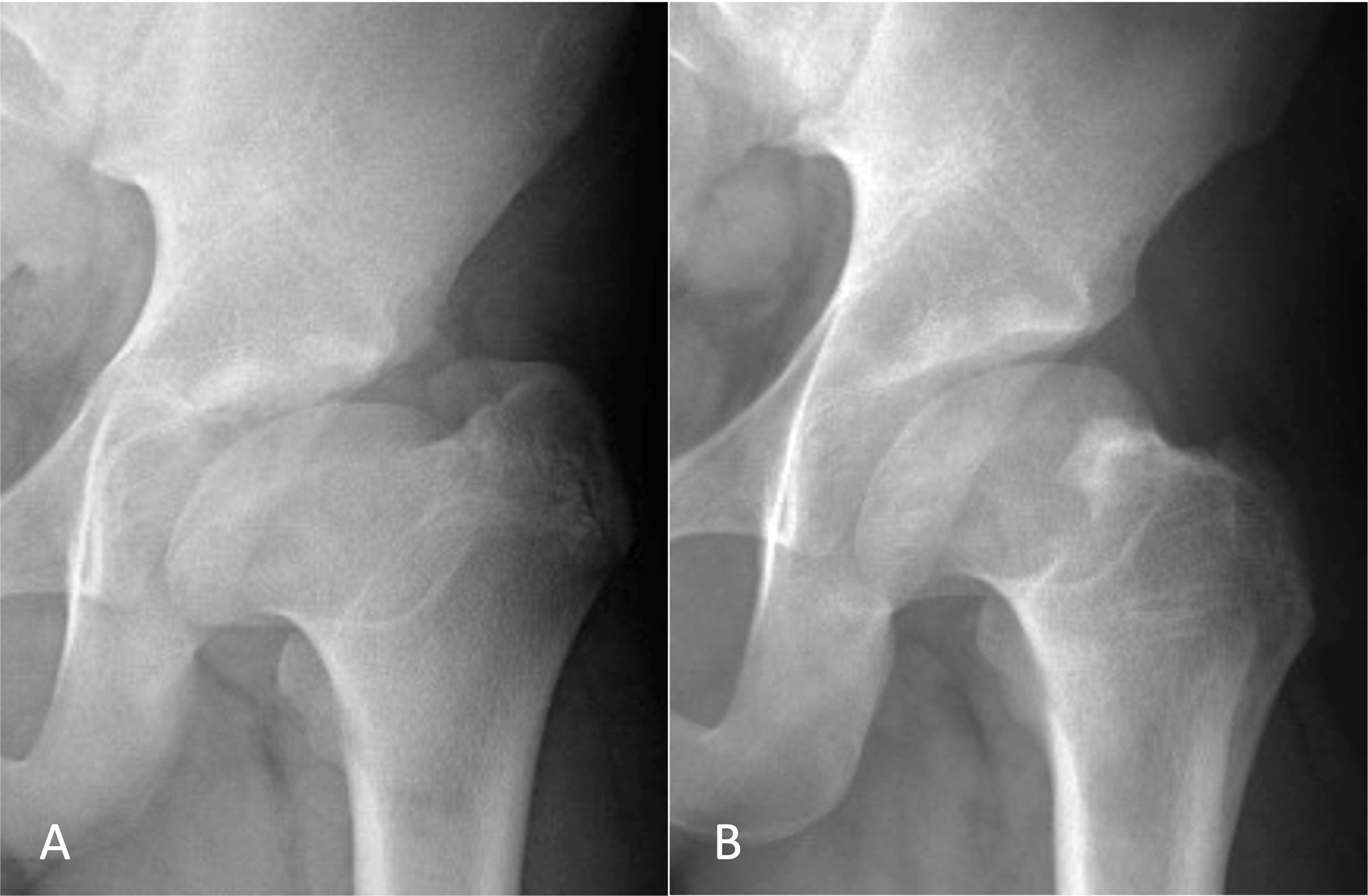
Multivariable analysis found 2 independent factors associated with surgical failure: the severity of preoperative pain as assessed by the WOMAC pain scale (hazard ratio [HR] = 1.16; 95% CI = 1.03 to 1.30; p = 0.01) and the severity of preoperative deformity as assessed by the anteroposterior alpha angle (HR = 1.06; 95% CI = 1.01 to 1.11; p = 0.01).
Conclusions
The authors conclude, “SHD with relative femoral-neck lengthening and osteochondroplasty of the femoral head-neck junction decreased pain and symptoms of stiffness for most patients with symptomatic residual LCPD deformity.” They further note, “Although our findings offer orthopaedic surgeons and patients with symptomatic healed LCPD more data to consider when determining whether to proceed with hip-preservation surgery, further research with larger sample sizes is needed to establish the role of other procedures such as PAO [periacetabular osteotomy] and femoral-head reduction osteotomy, and to clarify the best surgical strategies to maintain satisfactory function for as long as possible in the native hip.”
Access the full report at JBJS.org: