Notable findings in pediatrics regarding the treatment of fractures, infection, early-onset scoliosis, and more are presented in the new JBJS Guest Editorial What’s New in Pediatric Orthopaedics. Here, we highlight the 5 most compelling studies, as selected by author Christina K. Hardesty, MD.
Trauma
Researchers investigated whether the time to treatment of supracondylar humeral fractures affected clinical outcomes in pediatric patients. A total of 472 patients were included; 435 underwent surgical treatment within 18 hours of presentation and 37 underwent treatment after 18 hours. No differences in postoperative complications, including malunion, nonunion, stiffness, infection, and nerve injury, were found between the groups, even when Type II Gartland fractures were excluded1.
A randomized controlled trial compared 2 treatments for distal radial buckle fracture with respect to pain and function in patients 4 to 15 years old. Of the 965 patients included, 489 received a bandage and 476 received rigid immobilization. The groups had equivalent pain at 3 days following treatment and demonstrated no differences in pain or function during the 6-week follow-up period2. These findings suggest “that we may be overtreating distal radial buckle fractures in children when we routinely utilize rigid immobilization,” says Guest Editorial author Dr. Hardesty, adding that this study “has the potential to change all our practices, providing children with less rigid immobilization for buckle fractures.”
Infection
A study assessed the utility of procalcitonin, a protein released by tissues in response to bacteria or other infection, as a biomarker for musculoskeletal infection in pediatric patients. Procalcitonin was compared with traditional biomarkers in 188 children and found to outperform white blood-cell count, C-reactive protein, and absolute neutrophil count. A procalcitonin level of >0.1 ng/mL predicted deep infection in 84.7% of cases. Combining procalcitonin with C-reactive protein, erythrocyte sedimentation rate, and temperature improved diagnostic accuracy to 89.4%3.
Upper Extremity
The Function after Adolescent Clavicle Trauma and Surgery (FACTS) study group evaluated clavicular remodeling in 98 adolescent patients with completely displaced fractures treated nonoperatively. The study authors reported a high remodeling rate and observed that remodeling continued even beyond adolescence. Complete or near-complete remodeling was demonstrated in 85% of patients <14 years old and 54% of patients ≥14 years old at the time of injury4.
Spine
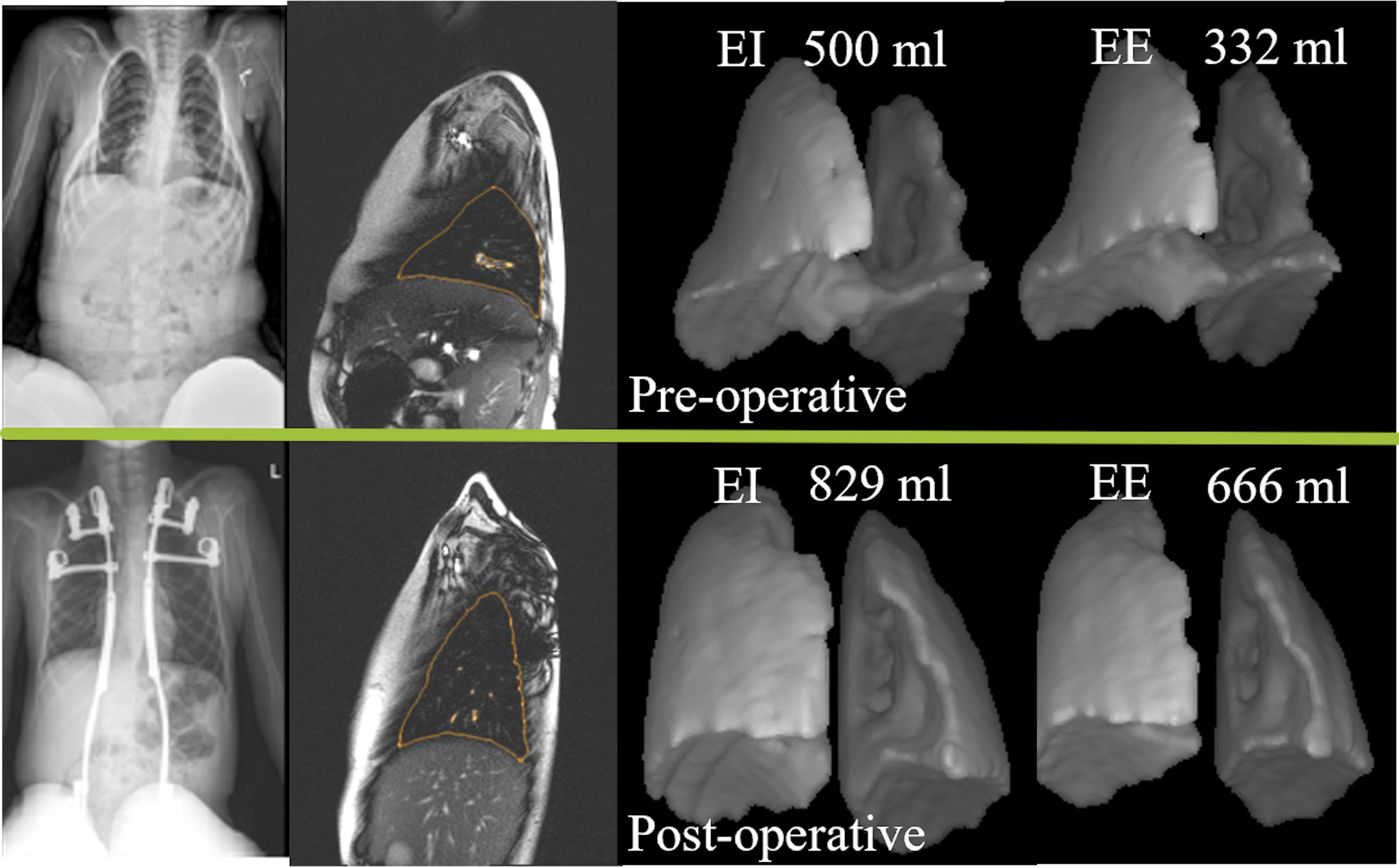
A Level II study published in JBJS utilized a novel dynamic MRI technique to evaluate pulmonary function in 39 patients treated surgically for thoracic insufficiency syndrome. Patients with thoracic insufficiency syndrome demonstrated improvement in tidal volumes and hemidiaphragm positions following the surgical procedure. Additionally, decreased deviation from normality was demonstrated in this group when their preoperative and postoperative parameters were compared with those of healthy children5.
What’s New in Pediatric Orthopaedics is freely available at JBJS.org.
What’s New by Subspecialty
Each month, JBJS publishes a review of the most pertinent studies from the orthopaedic literature in a select subspecialty. To read the reports, visit the What’s New by Subspecialty collection at JBJS.org.
Recent OrthoBuzz posts include: What’s New in Adult Reconstructive Knee Surgery, What’s New in Musculoskeletal Tumor Surgery, and What’s New in Musculoskeletal Basic Science.
Image modified from: Tong Y, Udupa JK, McDonough JM, Wu C, Sun C, Xie L, Lott C, Clark A, Mayer OH, Anari JB, Torigian DA, Cahill PJ. Assessment of Regional Functional Effects of Surgical Treatment in Thoracic Insufficiency Syndrome via Dynamic Magnetic Resonance Imaging. J Bone Joint Surg Am. 2023 Jan 4;105(1):53-62.
References
- Sullivan MH, Wahlig BD, Broida SE, Larson AN, Shaughnessy WJ, Stans AA, Milbrandt TA. Does shorter time to treatment of pediatric supracondylar humerus fractures impact clinical outcomes? J Pediatr Orthop. 2023 Jul 1;43(6):350-4.
- Perry DC, Achten J, Knight R, Appelbe D, Dutton SJ, Dritsaki M, Mason JM, Roland DT, Messahel S, Widnall J, Costa ML; FORCE Collaborators in collaboration with PERUKI. Immobilisation of torus fractures of the wrist in children (FORCE): a randomised controlled equivalence trial in the UK. Lancet. 2022 Jul 2;400(10345):39-47.
- van der Laan L, Gaines N, Van Horn N, Jo C, Ma Y, Copley LA. Comparison of procalcitonin with commonly used biomarkers and algorithms for evaluating suspected pediatric musculoskeletal infection in the emergency department. J Pediatr Orthop. 2023 Feb 1;43(2):e168-73.
- Pennock AT, Bastrom TP, Boutelle KE, Carroll AN, Edmonds EW, Nepple JJ, Polinsky SG, Spence DD, Perkins C, Willimon SC, Bae DS, Busch MT, Ellis HB, Hergott K, Kocher MS, Li Y, Pandya NK, Sabatini CS, Wilson PL, Heyworth BE; FACTS Study Group. Bony remodeling of adolescent displaced clavicle fractures: a FACTS study. Am J Sports Med. 2023 Mar;51(4):871-6.
- Tong Y, Udupa JK, McDonough JM, Wu C, Sun C, Xie L, Lott C, Clark A, Mayer OH, Anari JB, Torigian DA, Cahill PJ. Assessment of regional functional effects of surgical treatment in thoracic insufficiency syndrome via dynamic magnetic resonance imaging. J Bone Joint Surg Am. 2023 Jan 4;105(1):53-62.