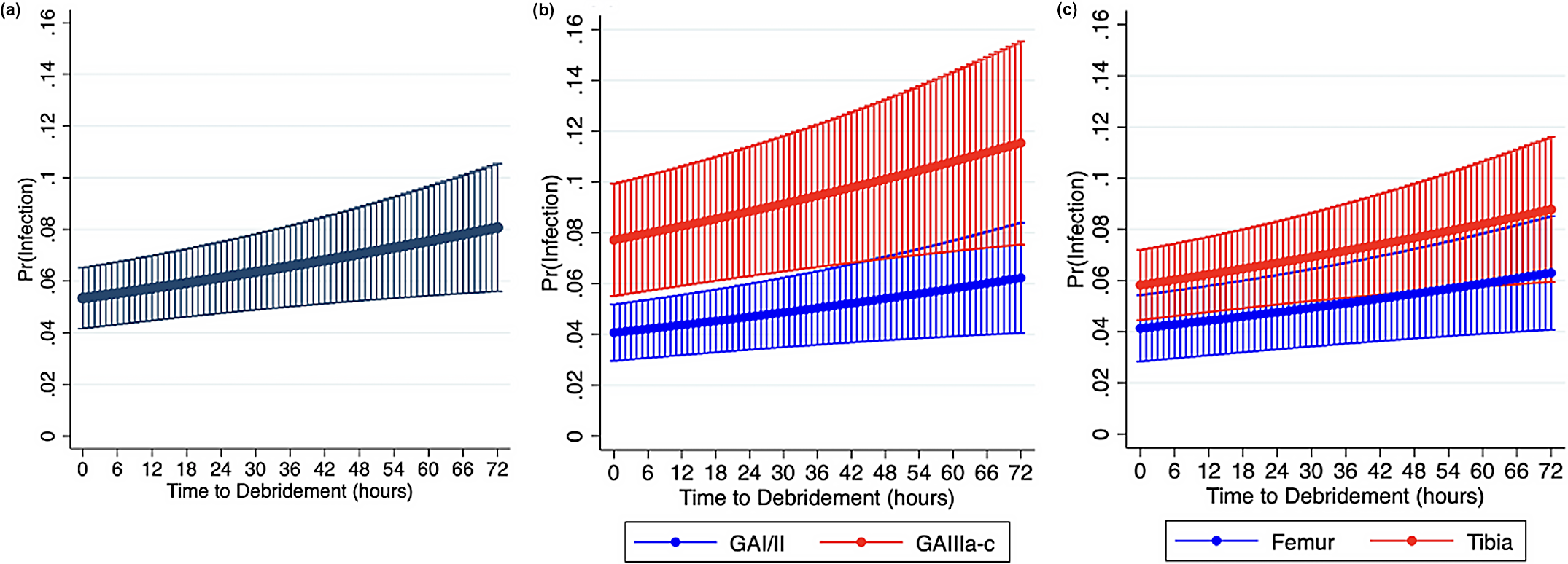
In this post, JBJS Editor-in-Chief Dr. Marc Swiontkowski discusses a new study on time to debridement of open femoral and tibial fractures and infection risk.
Category: Trauma

A new study in JBJS evaluates intramedullary fixation for femoral nonunion in pediatric patients in low- and middle-income countries. Dr. Matt Schmitz, JBJS Deputy Editor
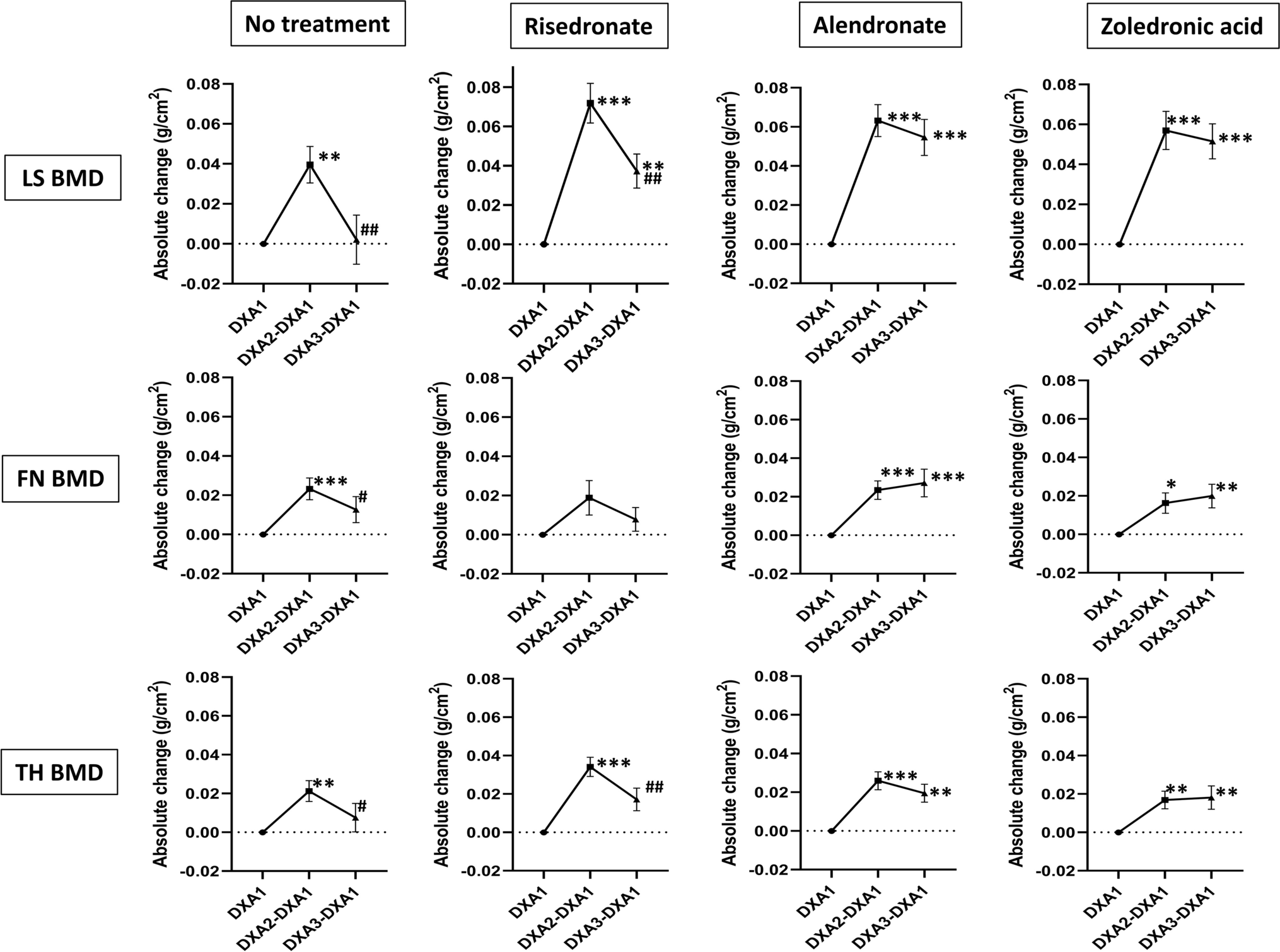
Vitamin D supplementation, fracture risk, and osteoporosis drug therapies are among several topics explored in recent studies featured in the new JBJS Guest Editorial: What’s
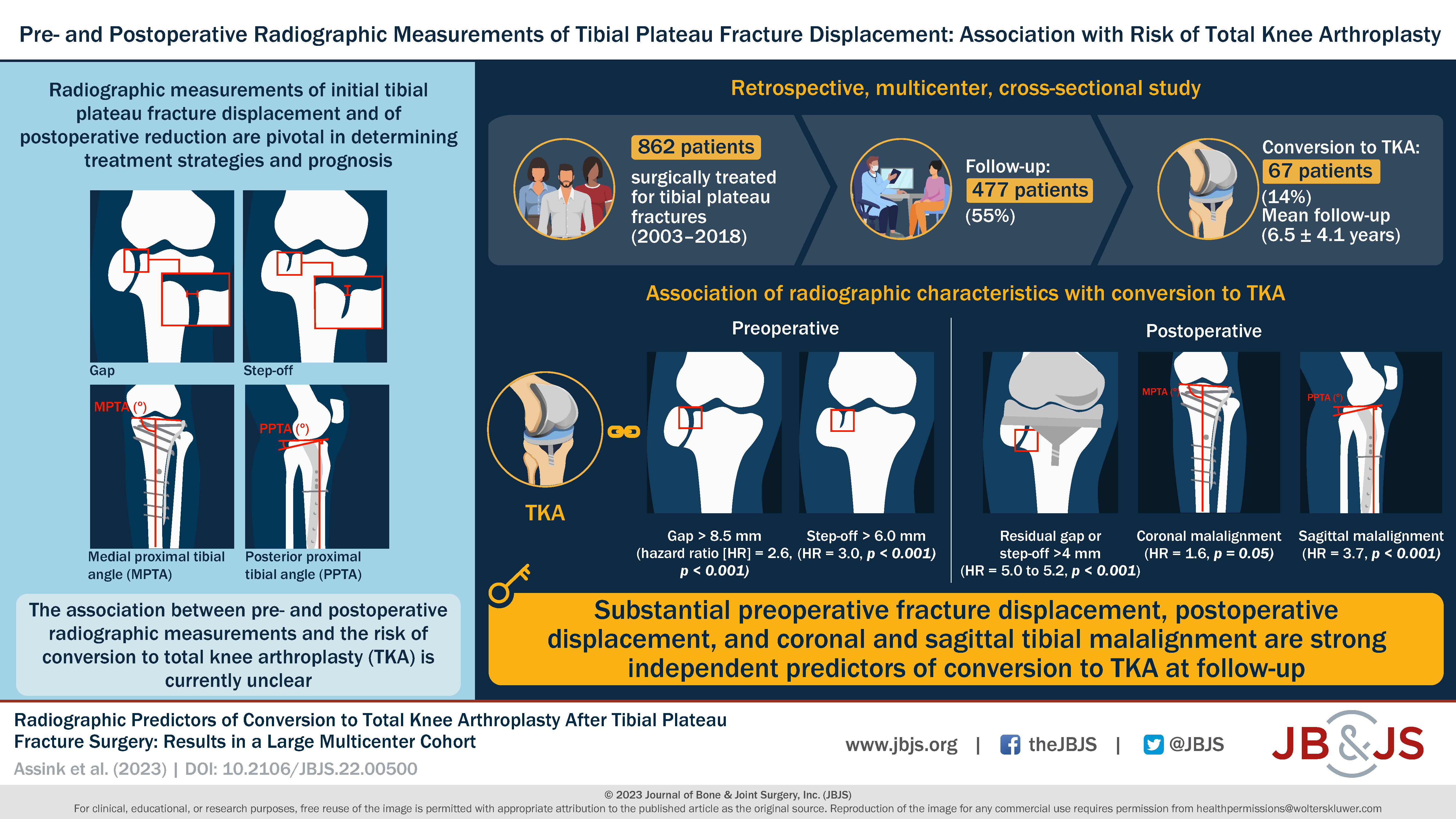
A new multicenter investigation by Assink et al. in JBJS explores the association between radiographic measurements and the risk of conversion to total knee arthroplasty
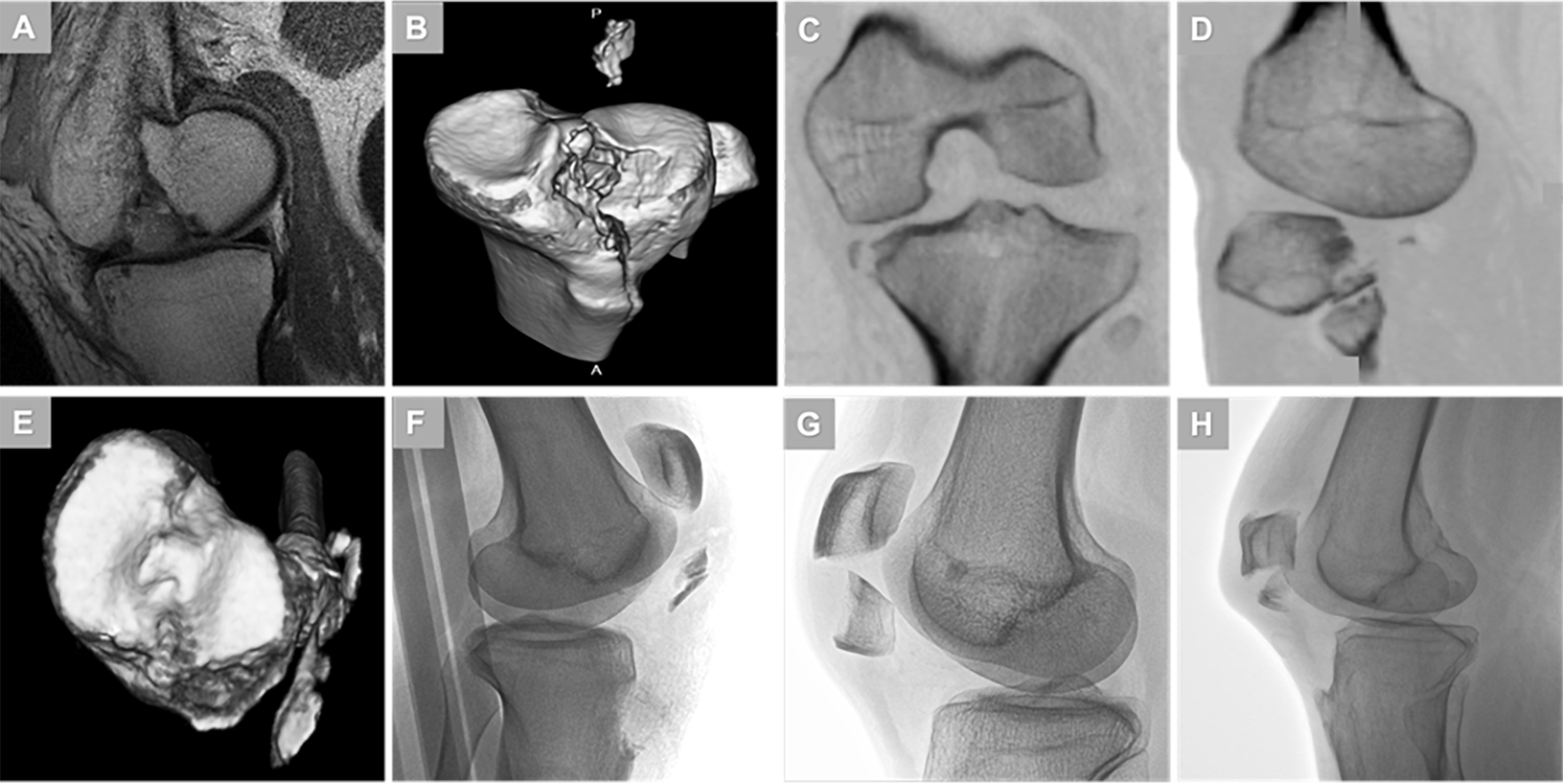
A new JBJS study establishes a consensus definition for fracture patterns within the Schenck Knee Dislocation V subcategory. Editor-in-Chief Dr. Marc Swiontkowski offers this perspective
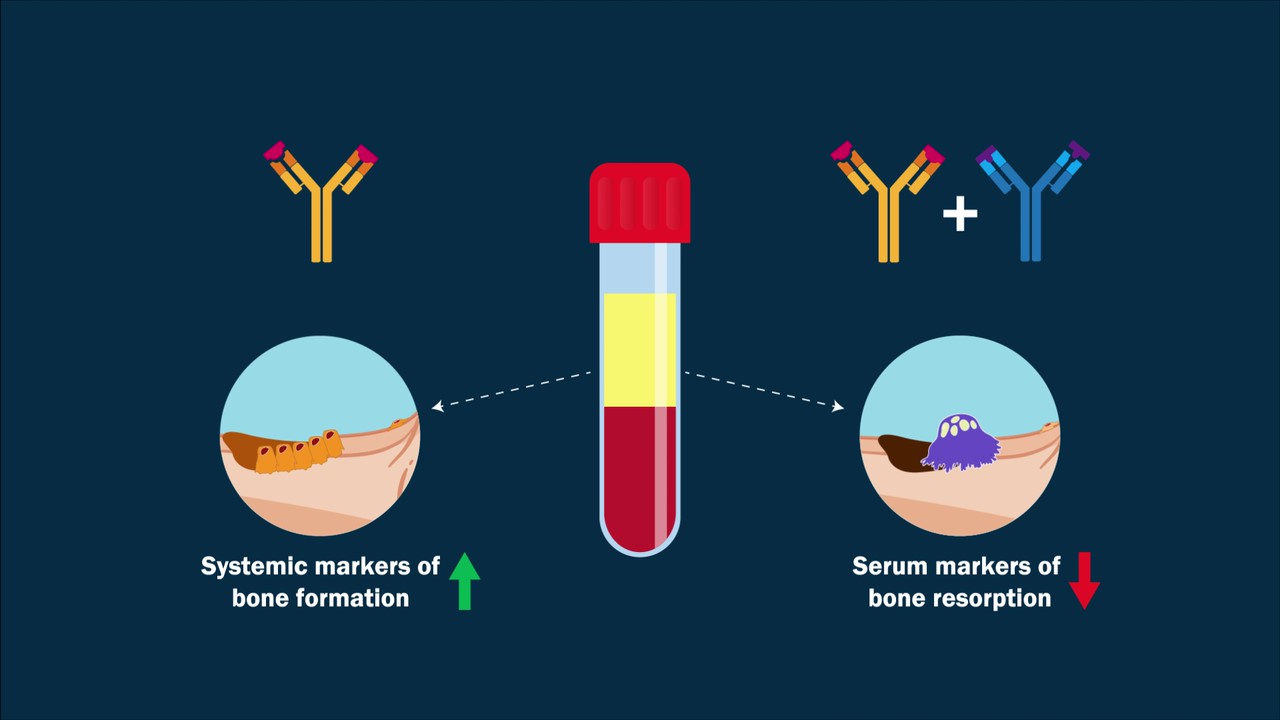
A video abstract is available with the new study by Florio et al. in JBJS: Dual Inhibition of the Wnt Inhibitors DKK1 and Sclerostin Promotes
Recent findings on fracture management and other trauma-related topics are presented in the new JBJS Guest Editorial “What’s New in Orthopaedic Trauma.” Here, we highlight
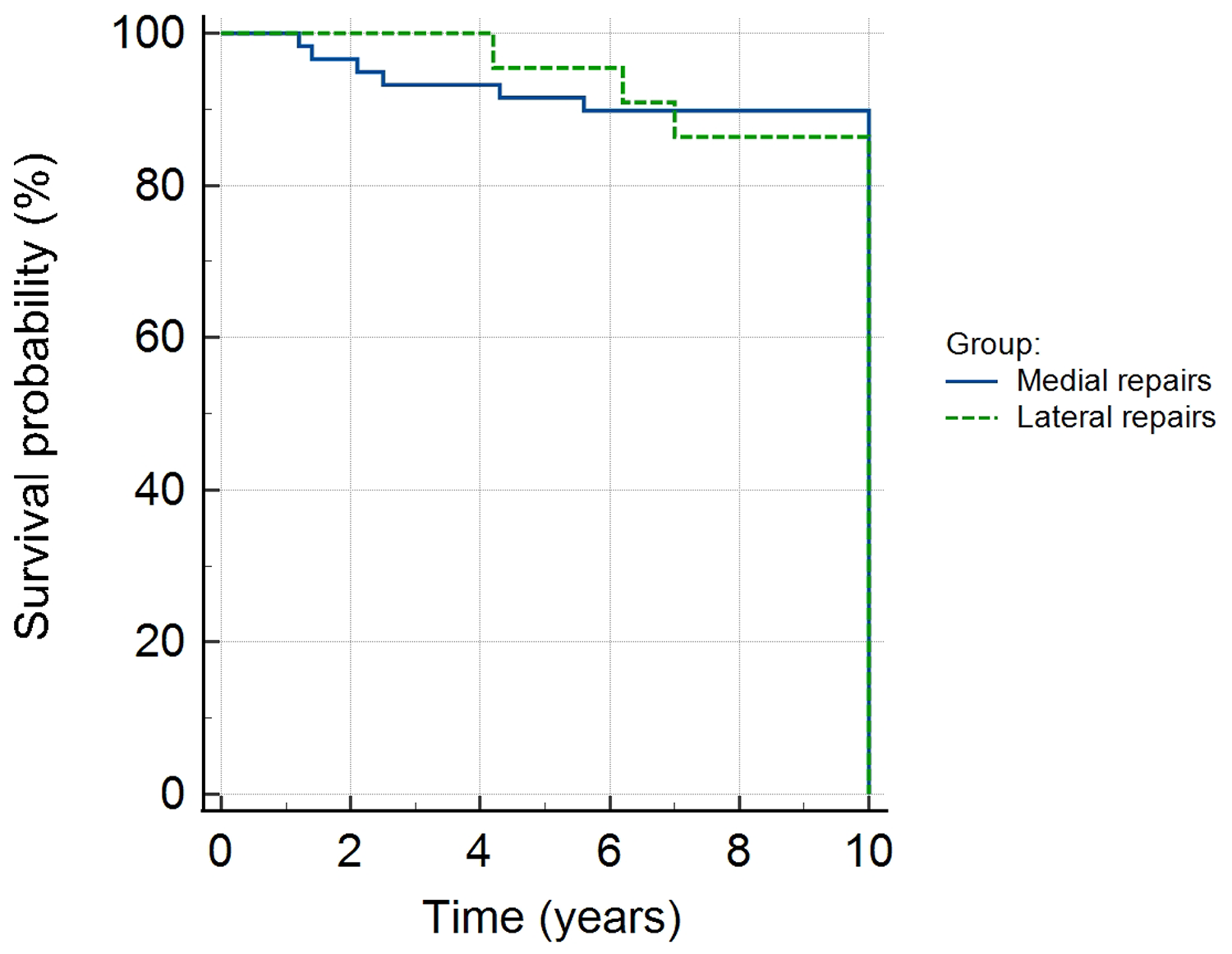
In this post, JBJS Deputy Editor for Social Media Dr. Matt Schmitz discusses a new study reporting 10-year outcomes of second-generation, all-inside meniscal repair with

This Resident Roundup post comes from Sean Pirkle, MD, a second-year resident with the Department of Orthopaedics and Sports Medicine at the University of Washington,
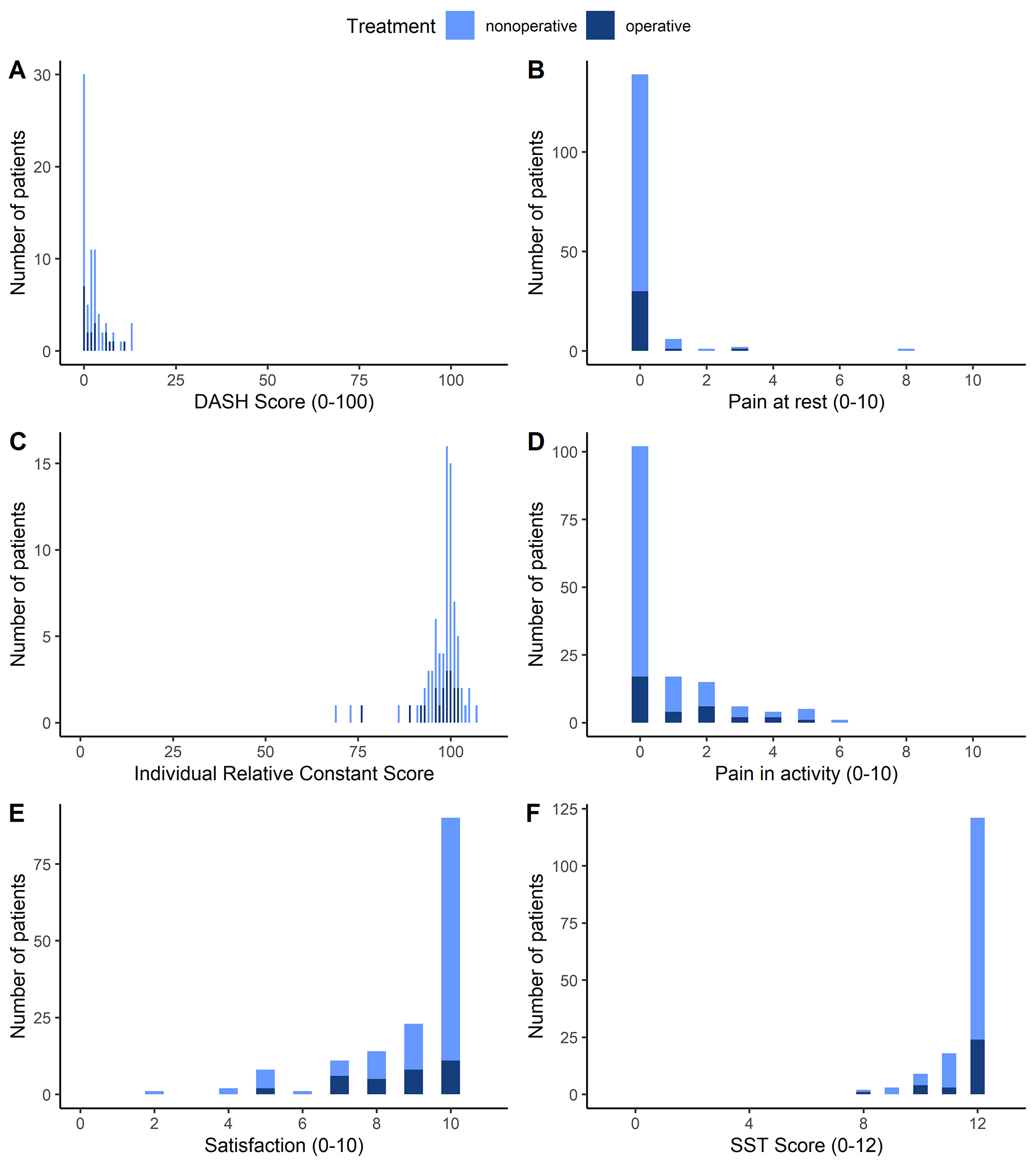
Dr. Marc Swiontkowski, JBJS Editor-in-Chief, discusses a new study assessing the long-term outcomes of proximal humeral fractures sustained in adolescence. Treating fractures involving the physes